“A COMPARATIVE STUDY ON THE EFFECTIVENESS OF SPECIFIC BALANCE STRATEGY VERSUS CONVENTIONAL BALANCE TRAINING TO IMPROVE BALANCE IN MULTIPLE SCLEROSIS PATIENTS – A RANDOMIZED CONTROLLED TRIAL.” – Dr. Arushi Tandon
“A COMPARATIVE STUDY ON THE EFFECTIVENESS OF SPECIFIC BALANCE STRATEGY VERSUS CONVENTIONAL BALANCE TRAINING TO IMPROVE BALANCE IN MULTIPLE SCLEROSIS PATIENTS – A RANDOMIZED CONTROLLED TRIAL.”
Dr. Arushi Tandon, B.P.T, Dr. Pragya Bhatt, M.Sc Anatomy (Medical)
ABSTRACT
BACKGROUND: Multiple sclerosis happens to be the most common neurological affliction among adults between the age of 20 and 40, with over 40,000 cases in India. MS in this series affects patients of all communities and different dietary habits. It is more common in the higher socioeconomic group. Patients with MS participate in exercise programmes to improve their balance but no study has investigated a specific balance strategy training intervention presented in a workstation format for small groups.
OBJECTIVE: to compare whether a specific balance strategy training programme delivered in a workstation format was superior to a conventional exercise programme for improving balance in patients with MS.
METHODOLOGY: after satisfying inclusion and exclusion criteria the subjects were randomly selected and assigned to two groups, group 1(conventional group) consisting of
15 patients which received conventional therapy which includes gentle stretches, co ordination exercises, strengthening exercises for lower limbs, controlled mobility exercises and biofeedback mirror. Group 2(experimental group) consisting of 15 patients which received specific balance strategy which includes several workstation tasks which are designed to improve functional abilities, improve upper and lower limb strength, teach multi tasking and provide vestibular stimulation along with the conventional therapy mentioned above. The treatment was given 4 days a week for 3 weeks.
RESULTS: all participants significantly improved in their balance (P<0.0000). The specific balance strategy intervention group showed significantly more improvement in functional measures than the control group (P=0.00341) with respect to BBS. Separate group analyses indicated slight to no improvement in performance in timed gait (P=0.710) with respect to timed up and go. The control group as well as the experimental group showed improvement in TUG.
CONCLUSION: the results provide evidence that all participants achieved a significant improvement in balance. Specific balance strategy training using workstations is superior to traditional exercise classes for improving function and balance.
KEY WORDS: randomised controlled trial, balance, functional ability, exercise, workstations, multiple sclerosis.
TABLE OF CONTENTS
| SL NO | TITLE | PAGE NO |
| 1 | Introduction | 1-10 |
| 2 | Objectives | 11-12 |
| 3 | Review of literature | 13-20 |
| 4 | Materials and Methodology | 21-27 |
| 5 | Results | 28-42 |
| 6 | Discussion | 43-46 |
| 7 | Conclusion | 47 |
| 8 | Summary | 48 |
| 9 | Bibliography | 49-53 |
| 10 | Annexure | 54-62 |
LIST OF TABLES
| SL
NO |
TABLE | PAGE |
| 1 | Inter group comparison of age of patients | 30 |
| 2 | Inter group comparision of age of the patients. | 31 |
| 3 | Inter group comparison of gender of the patients. | 33 |
| 4 | Intra group comparison with to the Berg balance
scale. |
35 |
| 5 | Inter group comparison of the Berg balance scores | 36 |
| 6 | Intra group comparison with the Timed up and go
scores |
38 |
| 7 | Inter group comparison with the timed up and go
test. |
39 |
| 8 | Gender and its effect on the outcome tools. | 41 |
| 9 | Age and outcome tools. | 42 |
LIST OF FIGURES
| Sl No | Title | Page |
| 1 | List of Pictures
Normal nerve and demyelinated nerve Subtypes of Multiple sclerosis MRI of brain affected with multiple sclerosis Tools used for the study Conventional set of exercises Hip extension being performed by the patient Forward reaching task The specific balance strategy exercises. List of Graphs Age groups of the patients in the experimental and control group. Different gender in both the groups. Pre and post test comparison for both the groups with berg balance scale Pre and post test comparison for both groups with timed up and go test. |
2 |
| 2 | 4 | |
| 3 | 6 | |
| 4 | 23 | |
| 5 | 24 | |
| 6 | 25 | |
| 7 | 25 | |
| 8 | 26 | |
| 1 | 32 | |
| 2 | 34 | |
| 3 | 37 | |
| 4 | 40 |
INTRODUCTION
Multiple sclerosis is an unpredictable disease that varies greatly from one individual to another in term of clinical presentation and the severity of symptoms presented. The onset typically occurs between the ages of 15 to 55 years, with the peak in the third decade. The disease is rare in children, as is the onset of symptoms in adults over the age of 50 years 1.
The prevalence of MS in India is low, and it is unclear whether the manifestations of the disease in India are similar to the United States. It happens to be the most common neurological affliction among adults between the age of 20 and 40, with over 40,000 cases in India, according to the survey done by India today magazine, 27th April 2009 issue. No Indian patient had a family history of MS; this suggests an environmental disease-triggering agent 2. The calculations based on the hospital data suggest an approximate prevalence rate of 0.17 to 1.33 per 100,000 of population in different parts of India. The incidence in females is twice that in males. The optico-spinal form of MS is the commonest (71.4%) in India. Multiple sclerosis in this series affects patients of all communities and different dietary habits. MS is more common in the higher socioeconomic group whereas neuromyelitis optica, a similar condition, is mainly seen in patients in the low socioeconomic group 3.
Multiple sclerosis is defined as, a progressive disease characterized by disseminated demyelination of nerve fibres of the brain and spinal cord. Begins slowly, usually in young adulthood continues throughout life with periods of exacerbation and remission 1. Clinically MS is characterised by multiple signs and symptoms and fluctuating periods of exacerbation and remission. An exacerbation involves a relapse or
period of symptom flare up, whereas a remission is a period free of evolving symptoms. The course of the disease is highly unpredictable. In the early stages, relatively complete remission of initial symptoms may occur; however, as the disease progresses, the remissions may become less complete with increased neurological dysfunction and complications that affect multiple body systems 1.
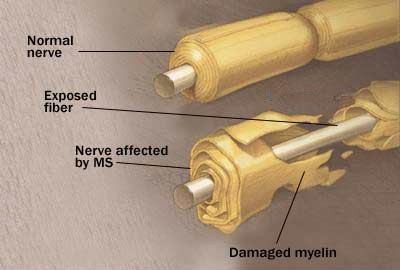
Fig.1 Normal nerve and demyelinated nerve
Conduction through the myelinated pathways in the central nervous system is saltatory, individual axons transmitting fast trains of impulses. Myelin injury blocks conduction and although function may be preserved by redundancy in individual systems or tracts, strategically placed pathways may lose their safety margin, resulting in neurological symptoms and signs as seen in Multiple sclerosis 4.
Viral infections trigger the production of lymphocytes (T cells, B cells) and macrophages, which in turn appear to produce cytotoxic effects within the central nervous system. Reactive astrogliosis results in destruction of oligodendrocytes (myelin-
producing cells) and the myelin sheath that surrounds the nerve. Disruption of the myelin sheath (demyelination) slows neural transmission and causes nerve to fatigue rapidly. With severe disruption, conduction block occurs with disruption of function. Local inflammation, oedema and infiltrates surround the acute lesion and cause a mass effect, further interference with the conductivity of the nerve fibre. During the early stages of MS, remaining oligodendrocytes may survive the initial insult and produce remyelination. As the disease becomes more chronic, no oligodendrocytes are preserved, and remyelination does not occur. The demyelinated areas eventually become filled with fibrous astrocytes and undergo a process called gliosis. Gliosis refers to the proliferation of neuroglial tissue within the CNS those results in glial scars (plaques). They primarily affect white matter, although lesions in grey matter are seen in advanced disease1.
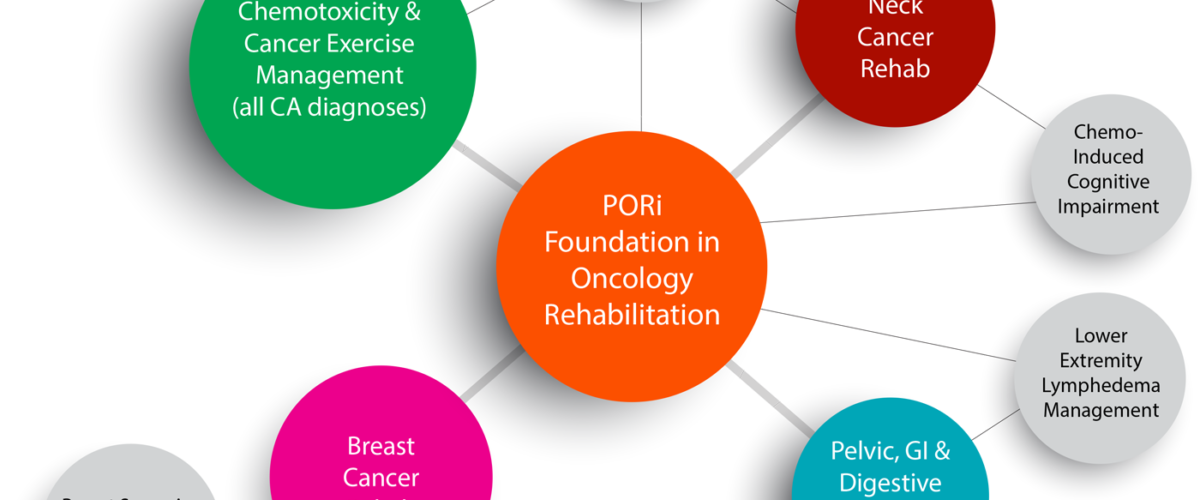
In 1996 the United States National Multiple Sclerosis Society standardized four subtype definitions;
Relapsing remitting Secondary progressive Primary progressive Progressive relapsing
Fig.2 Subtypes of Multiple sclerosis.
Partially demyelinated axons may discharge spontaneously, thus accounting for many unpleasant distortions of sensation reported by a high proportion of patients. Increased mechanical sensitivity manifests as movement induced symptoms, including flashes of lights provoked by eye movement and the electric sensation that spreads down the spine, limbs or anterior chest wall after neck flexion-Lhermitte’s sign 4.
Therefore most frequent symptoms of MS being 5
Fatigue-88%
Walking problems-87%
Bowel and bladder problems-65% Pain and other sensations-60% Visual disturbances-58% Cognitive problems-44% Tremors-41%
Multiple sclerosis can be difficult to diagnose since its signs and symptoms may be similar to many other medical problems. Medical organizations have created diagnostic criteria to ease and standardize the diagnostic process for practicing physicians. Currently, the McDonald criteria focus on a demonstration with clinical, laboratory and radiologic data of the dissemination of MS lesions in time and space. Most commonly used diagnostic tools are neuroimaging, analysis of cerebrospinal fluid and evoked potentials. Magnetic resonance imaging of the brain and spine shows areas of demyelination (lesions or plaques). There are certain areas of predilection, such as the optic nerve, sub cortical (especially periventricular) white matter, corticospinal tracts, posterior white column of the spinal cord and cerebellar peduncles. Testing of cerebrospinal fluid obtained from a lumbar puncture can provide evidence of chronic inflammation of the central nervous system. The cerebrospinal fluid is tested for oligoclonal bands, which are an inflammation marker found in 75% to 85% of people with MS. The nervous system of a person with MS often responds less actively to stimulation of the optic nerve and sensory nerves due to demyelination of such pathways. These brain responses can be examined using visual and sensory evoked potentials 17.
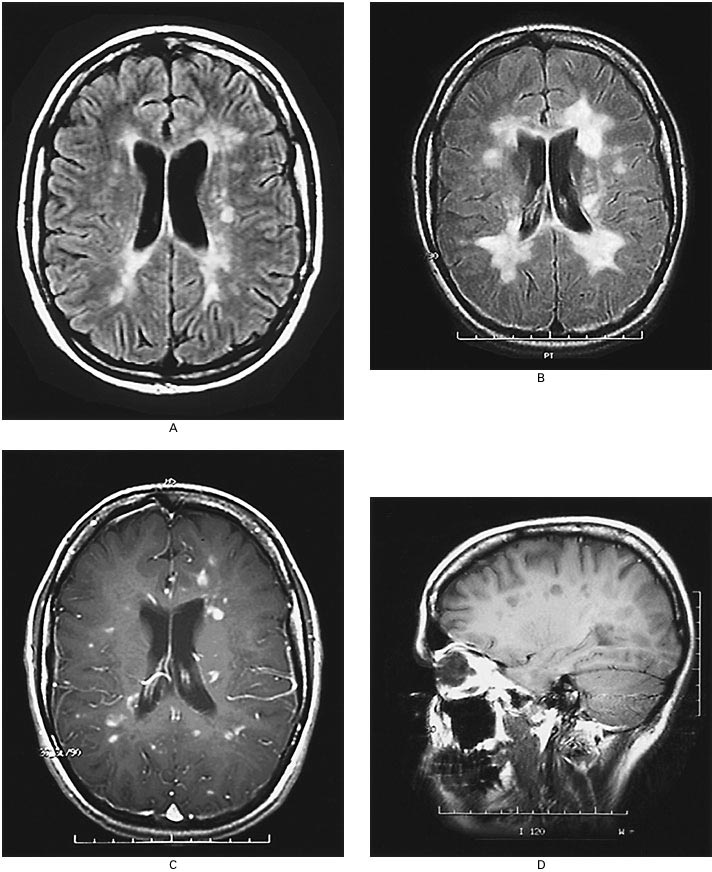
Fig.3 MRI of brain affected with multiple sclerosis.
Abnormalities in balance control are common findings in people with multiple sclerosis and can along with other risk factors increase risk of falls. These abnormalities, together with other impairments and disabilities, often prevent people from performing their daily living activities. In the past decade much attention has been directed towards the rehabilitation of balance in elderly people. Recently the assessment and the treatment of balance and gait impairments in multiple sclerosis have gained more interest within the scientific community7. Patients with multiple sclerosis fall inside their homes and outside in the community. They show a decline in ability to maintain balance when faced with the
perturbations imposed by functional requirements such as dividing attention between tasks as is needed to keep balance when walking in a crowd or on a busy road crossing. Declines in sensory (vision, vestibular and proprioception) and motor (strength, coordination, endurance) function and integration (response time, multi-task ability) have been identified as the major intrinsic factors contributing to falls 8, 10-15.
Keeping the body in balance involves many messages going to and from the brain. Even standing still, the body is constantly adjusting to the environment and making tiny changes. Multiple sclerosis causes damage to the many areas of the central nervous system that can impact postural responses to maintain balance, including the cerebellum and spinal cord 9. Cerebellar problems are common in MS. Balance and co ordination problems predispose the individuals to falls. Ataxia, in coordination, dysmetria and tremor that become exaggerated with movement may be present in all the extremities and trunk 6.
Spasticity can have a significant impact on function in MS patients. It can accompany weakness or interfere with functions despite relative normal strength. It coexists with weakness and may present as phasic spasms or sustained increase in tone. Spasticity can interfere with mobility and may also cause pain, predispose the individual to contractures and lead to poor postures 6. Weakness is a common finding in individuals with MS and a frequent cause for impairment. With lower extremity involvement, patients will typically describe worsening balance during ambulation and the need to hold on to walls or furniture.
During ambulation, patients will typically display a wide based gait with worsening balance when initiating gait or changing direction. The proximal muscles and the trunk muscles are much more frequently involved in MS which results in loosing balance during the day to day activities 16. Decreased strength results from several causes:
upper motor neuron weakness, fatigue, disuse, compensatory movements, pain and overriding spasticity in an antagonistic muscle. Pain frequently associated with MS is caused by spasticity, poor posture or abnormal use of muscles to compensate for loss of function. Contractures, disuse atrophy, decubitus ulcer and risk of falls and loss of balance are known complications of MS leading to increased dependency 6.
The primary aims of the therapy are returning functions after an attack, preventing new attacks and preventing disabilities. Both drug therapy and neuro-rehabilitation have shown to ease the burden of some symptoms, even though neither influences disease progress. A multidisciplinary approach is the key to limiting and overcoming disabilities10.
In physical therapy, conventional therapies given for balance includes, static holding in different weight bearing positions, progression through series of postures, joint approximation techniques and rhythmic stabilization(Proprioceptive Neuromuscular Facilitation),controlled mobility activities, strengthening the fixating muscles, visual cues, Swiss ball exercises , Frenkels exercises etc 1.
Previous research has shown that exercise such as strength, flexibility, balance training, Tai Chi and combinations of these activities delivered in a class situation or individually have increased strength, improved balance and improved functional ability in addition to reducing risk of falls. A multi-focus rather than a sole physical intervention approach appears to be superior in reducing falls. Thus, including fall prevention education, home evaluation and modification, medical review of physical status and medication in conjunction with an exercise programme has been shown to be most beneficial 8.
In this experimental approach, each workstation is designed to focus on a specific task that addresses aspects required for balance including functional strength, flexibility, balance strategy practice, sensory integration, and added attention demands during function and multi-task practice. Each station task is graded to cater to various levels of ability so that participants can have the level of difficulty progressed to increase the challenge. This versatility of degree of difficulty also allows for accommodation to various levels of ability of individual participants. In the workstation situation, the physiotherapist positions to ensure safety. Another advantage of the workstation application is the encouragement of self-efficacy in the participants who take control of their programme by remembering what task to practise and how to increase the challenge at each station after consultation with the physiotherapist 8.
Berg balance scale and time up and go test have acceptable concurrent validity in testing static and dynamic stability in individuals with multiple sclerosis 41, 42.
Recent evidence supports that specific balance strategy training using workstations is studied, to be effective for improving function and balance 8. No previous studies have investigated the efficacy of a specific balance strategy-training programme presented through a workstation or circuit programme as the exercise intervention for improving the balance in people with multiple sclerosis. This study focuses to evaluate the effects of balance retraining in a population of people with multiple sclerosis with this specific balance strategy.
NEED FOR THE STUDY
Multiple sclerosis happens to be the most common neurological affliction among adults between the age of 20 and 40 and most common cause of disability among the adults & makes an important contribution to the morbidity, mortality and disability in developing as well as developed countries. Very fewer studies have investigated the efficacy of a particular set of balance programme as the strategy to improve balance in multiple sclerosis. No study has been done to find the efficacy of the specific balance strategy-training programme as the exercise intervention in multiple sclerosis patients. Therefore the need of the study arises to compare the effectiveness of specific balance training strategy with conventional balance exercises in multiple sclerosis patients.
OBJECTIVE OF THE STUDY
- To evaluate the effects of specific balance strategies in multiple sclerosis patients.
- To evaluate the effects of conventional balance strategies in the multiple sclerosis patients.
- To compare the efficacy of specific balance strategies over the conventional balance strategies.
HYPOTHESIS:
Experimental Hypothesis:-
The specific balance strategy may have a significant result in regaining balance in multiple sclerosis patients than the conventional balance strategies.
Null Hypothesis:-
The specific balance strategy may not have a significant result in regaining balance in multiple sclerosis patients than the conventional balance strategies.
MATERIALS AND METHODOLOGY
Source of data:
- Justice K.S.Hegde Charitable Hospital, Deralakatte, Mangalore.
- Private clinics (Physiotherapy) from Mangalore and Bangalore
Sampling procedures:
By using randomised sampling techniques
Design:
Randomized Experimental study design.
Subjects: Thirty patients with multiple sclerosis satisfying the inclusion criteria were selected for the study.
Group 1: Consisting of 15 patients who received conventional therapy which includes gentle stretches, co ordination exercises, strengthening exercises for lower limbs, controlled mobility exercises and biofeedback mirror.
Group 2: Consisting of 15 patients who received specific balance strategy which includes several workstation tasks which are designed to improve functional abilities, improve upper and lower limb strength, teach multi tasking and provide vestibular stimulation along with the conventional therapy mentioned above.
Method of Collection of Data:
SUBJECT SELECTION CRITERIA
Inclusion criteria
- Multiple sclerosis with motor balance disorders
- Relapsing – remitting type of multiple sclerosis.
- Ability to stand independently for more than 30 sec and ability to walk for 6m.[7]
- 25-55 age
- Both females and males
Exclusion Criteria
- Medically unstable patients.
- Non co-operative.
- Severe sensory involvement or sensory ataxia.
- Any musculoskeletal deformities.
- Vestibular involvement
- Peripheral nerve involvement.
- Progressive type of multiple sclerosis
Materials:-
-
- Chair
- Cup and saucer
- Mirror
- Soft mat
- Small objects like balls, toys etc
- Blocks of different heights tables
- Inflated beach balls, hard balls
- Pack of cards
- Ankle cuffs
Fig 4 Materials used. Ankle cuff, balls, cup and saucer and pack of cards.
OUTCOME TOOLS
-
- Timed up and go test.
- Berg balance scale.
Procedure :
30 patients were selected by using randomized controlled technique after fulfilling the criteria from the population and then divided into two groups. Each group consist of 15 patients. A written consent was taken from the patient after explaining about the intervention procedure and ethical clearance was obtained from the ethical committee of K S Hegde Medical Academy.
The mean ages in both the groups were 38. The maximum numbers of patients (26.7%) were in the age group 51-55. Equal number of males (7) and females (8) were taken in both the experimental and control group.
Group 1 received conventional balance training which includes gentle stretches, coordination exercises, strengthening exercises for lower limbs, controlled mobility exercises and biofeedback mirror.
The conventional exercises are explained below 8:
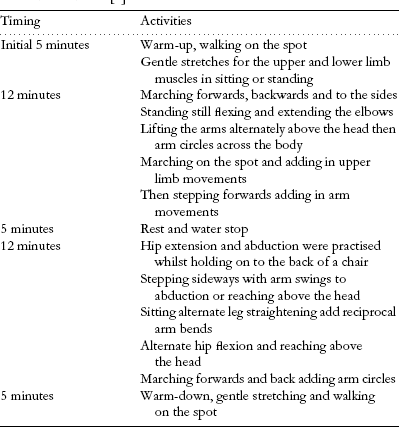
Fig.5 table showing conventional set of exercises.
Balance progressed with easiest (with support) to most difficult (without support). The interventions were given for 45 minutes a day for 4 days a week and for 3 weeks with adequate rest period 7.
Fig 6: Hip extension being performed by the patient, part of the conventional balance exercise.

Fig 7: Forward reaching task, part of the specific balance strategy, being performed by the patient.
Group 2 received specific balance strategy which included several workstation tasks which were designed to improve functional abilities, improve upper and lower limb strength, teach multi tasking and provide vestibular stimulation 8
The workstations are explained in the table below 8:

Fig.8 The specific balance strategy exercises.
These exercises are progressed gradually, the progression is made when subject performs task easily without any loss of balance. The interventions were given for 45 minutes a day for 4 days a week and for 3 weeks with adequate rest period 7.
Before and after the intervention for both the groups’ pre and post test score will be obtained for the balance using berg balance scale and timed up and go test. Berg balance test is a 14 item scale designed to measure balance of the adults in a clinical setting. It consists of a 5 point ordinal scale, ranging from 0-4. “0” indicates the lowest level of function and “4” the highest level of function. Total Score = 56. Authors support a cut off score of 45/56 for independent safe ambulation. The drawback of this scale is that it does not include gait item. Timed up and go test is a test for basic functional mobility. Normal healthy elderly usually complete the task in ten seconds or less. Very frail or weak elderly with poor mobility may take 2 minutes or more. Results correlate with gait speed, balance, functional level, the ability to go out, and can follow change over time.
DATA ANALYSIS AND RESULTS:
The data of the improvement in the balance within both the groups were analysed with the help of paired “t” test. The inter group analysis was done with the help of unpaired “t”test. For comparing the scores obtained with the timed up and go test within the groups Wilcoxon signed rank test was used and for inter group analysis Mann- Whiteny U test was used. The formulae of the tests used are as follows:
- Paired “t” test:
∑ = Sum 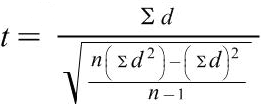
n = sample size
d = difference between variables
- Unpaired “t” test
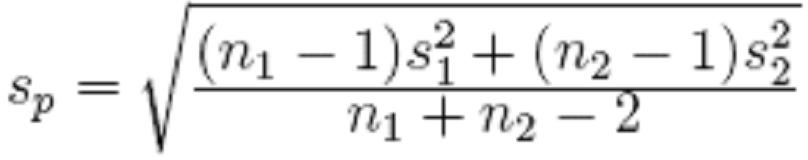
For experimental group, group 1 Sample size= n1
Sample mean= x1
Sample stadard deviation= s1 For control group, group 2 Sample size= n2
Sample mean= x2
Sample stadard deviation= s2
- Wilcoxon signed rank test.
![]() (W— W)±.5
(W— W)±.5
z =
![]() W
W
Where,
W= sum of signed ranks
µw = 0
![]() w= variable of the signed ranks.
w= variable of the signed ranks.
- Mann – Whitney U test
U1 = n1 .n2 + n1(n1+1) – R1
2
Where n1 is the two sample size for sample 1, and R1 is the sum of ranks in sample 1 U2 = n1 .n2 + n2(n2+1) – R2
2
Where n2 is the sample size for sample 2, & R2 is the sum of the ranks in sample 2 The sum of the two values is then given by
U1 + U2 = n1.n2 + n1 (n1+1) – R1+ n1.n2 + n2 (n2+1) – R2
2 2
Where,
n1 = sample size for control group
n2 = sample size for experimental group R1 = sum of ranks in control group
R2 = sum of ranks in experimental group U = Mann- Whiteny U test value.
Table 1
Inter group comparison of age of patients
| Group | Total | |||
| Experimental | Control | |||
| Age | 21 – 25 | 0
.0% |
2
13.3% |
2
6.7% |
| 26 – 30 | 1
6.7% |
1
6.7% |
2
6.7% |
|
| 31 – 35 | 2
13.3% |
2
13.3% |
4
13.3% |
|
| 36 – 40 | 2
13.3% |
2
13.3% |
4
13.3% |
|
| 41 – 45 | 3
20.0% |
2
13.3% |
5
16.7% |
|
| 46 – 50 | 3
20.0% |
2
13.3% |
5
16.7% |
|
| 51 – 55 | 4
26.7% |
4
26.7% |
8
26.7% |
|
| Total | 15
100.0% |
15
100.0% |
30
100.0% |
|
Table 1 shows the different ranges of the age of the patients. The mean age of the group is
38. Maximum percentages 26.7% of people lie in the age group of 51-55 in both experimental and control group.
Table 2
Inter group comparision of age of the patients.
| Group | N | Minimum | Maximum | Mean | Std.
Deviation |
Median | t value | p value |
| Age Experimental | 15 | 30 | 54 | 43.67 | 8.321 | 43.00 | .669 | .509 |
| Control | 15 | 23 | 55 | 41.27 | 11.119 | 45.00 | NS | |
| Total | 30 | 23 | 55 | 42.47 | 9.726 | 44.00 |
Table 2 shows inter group comparison with respect to age, 43.67 is the mean age in the experimental group and 8.321 is the standard deviation. In the control group mean age being 41.27 with a standard deviation of 11.119. With unpaired “t” test, the “t” value obtained was 0.669 with a p value 0.509. The p value is not significant this implies that the study is not biased with age factor.
Graph1 depicts that the maximum number of patients were of the age group 51-55 both in the experiment and control group. The least number of patients found were of the age group 26-30.
Graph 1
Age groups of the patients in the experimental and control group.
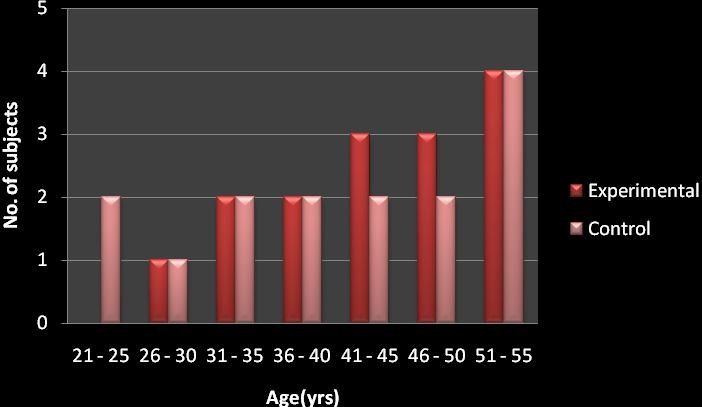
Table 3
Inter group comparison of gender of the patients.
| Group | Total | |||
| Experimental | Control | |||
| Sex | Female | 8
53.3% |
8
53.3% |
16
53.3% |
| Male | 7
46.7% |
7
46.7% |
14
46.7% |
|
| Total | 15
100.0% |
15
100.0% |
30
100.0% |
|
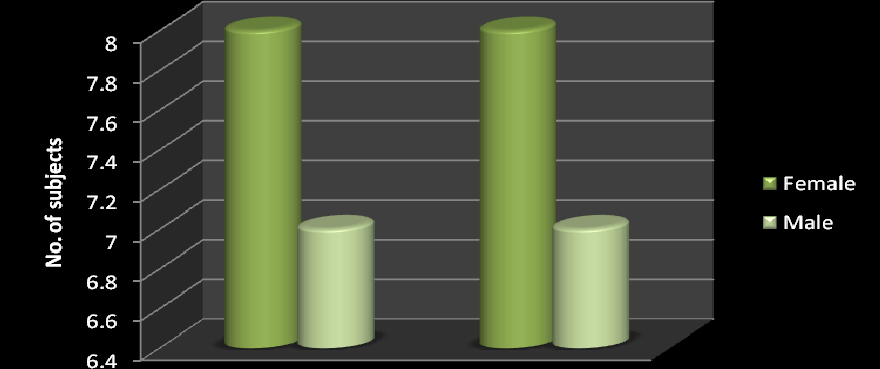
The table shows the inter group comparison of the gender of the patients. 53.3% of the patients being females and 46.7% being males in both experimental and control group. This implies that the study is not biased with the gender of the patients either.
Graph 2 depicts the same, showing equal number of females and males in both the experimental and control group.
Graph 2
Different gender in both the groups.
![]()
Table 4
Intra group comparison with to the Berg balance scale.
| Group | N | Min | Max | Mean | Std.
Deviation |
Median | Mean
Difference |
t
value |
p
value |
|
| Experimental | Pre
BBS |
15 | 19 | 42 | 30.87 | 5.167 | 30.00 | 5.4000 | 8.259 | .000 |
| Post
BBS |
15 | 28 | 49 | 36.27 | 5.351 | 35.00 | HS | |||
| Control | Pre
BBS |
15 | 28 | 35 | 31.40 | 2.324 | 30.00 | 3.000 | 5.434 | .000 |
| Post
BBS |
15 | 31 | 36 | 34.40 | 1.502 | 35.00 | HS |
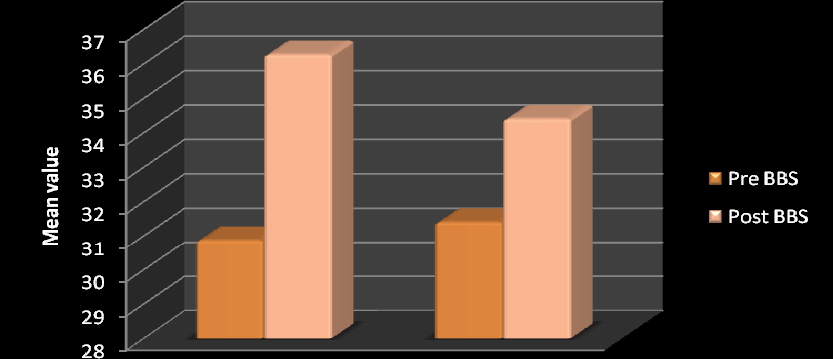
The experimental group receiving the specific balance strategy has shown improvement from a mean score of 30.87 to 36.27. Mean difference of improvement being 5.400. The t value is 8.259 and p value being 0.000. The control group also shows an improvement from 31.40 to 34.40. The mean difference here is 3.000. The t value is
5.434 and the p value is 0.000. Thus the statistics shows an improvement in both the experimental group and the conventional group in their pre and post scores.
Table 5
Table showing inter group comparison of the Berg balance scores
m
| Group | N | Minimum | Maximu | Mean | Std.
Deviation |
Median | t value | p vale |
| Effect(Pos Experime
Pre) BBS Control |
15
15 |
1
0 |
9
6 |
5.40
3.00 |
2.063
2.138 |
5.00
2.00 |
3.200 | .00341
HS |
The mean value in the experimental group is 5.40 and the mean value in the control group is 3.00 with a t value of 3.200 and p value of .00341. Thus the study shows a significant improvement in both the groups. But when the scores are compared with each other the experimental group score shows more improvement.
The graph 3 also denotes the same. In both the control and experimental the post intervention scores are higher than the pre. Showing a significant improvement, but the experimental group shows a better improvement in comparison to the control group.
Graph 3
Pre and post test comparison for both the groups with berg balance scale.
![]()
Table 6
Table shows intra group comparison with the Timed up and go scores
| Group | N | Minimum | Maximum | Mean | Std.
Deviation |
Median | Wilcoxon Signed Ranks Test
z value |
p vale |
| Experimen Pre TUG
Post TUG |
15
15 |
1
1 |
2
2 |
1.80
1.40 |
.414
.507 |
2.00
1.00 |
2.449 | .014
sig |
| Control Pre TUG
Post TUG |
15
15 |
1
1 |
2
2 |
1.73
1.40 |
.458
.507 |
2.00
1.00 |
2.236 | .025
sig |
The mean value of the timed up and go in the experimental group has shown an improvement from pre value of 1.80 to post value of 1.40 with a z value of 2.449 and p value of 0.014. The mean value of the same in the control group has shown an improvement from pre value of 1.73 to post value of 1.40 with a z value 2.236 and p value of 0.025. Thus both the group are showing significant improvement within, with respect to the timed up and go test.
Table 7
Inter group comparison with the timed up and go test.
| Group | N | Minimum | Maximum | Mean | Std.
Deviation |
Median | Mann- Whitney U test Z
value |
p vale |
| Effect(Post- Experiment
Pre) TUG Control |
15
15 |
0
0 |
1
1 |
.40
.33 |
.507
.488 |
.00
.00 |
.372 | .710
NS |
The mean value in the experimental group is 0.40 and in the control group is 0.33. The z value with the Mann Whitney U test is 0.372 giving a p value of 0.710. This shows that the interventions have not brought a significant result when compared between both the groups. The graph 4 indicates the same.
Graph 4
Pre and post test comparison for both groups with timed up and go test.
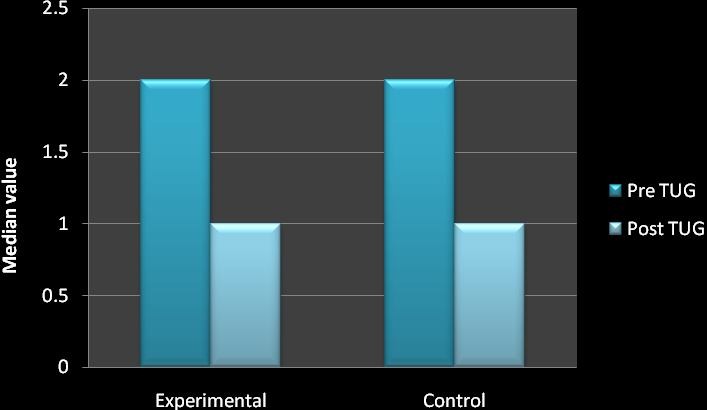
Table 8
Gender and its effect on the outcome tools.
| Group Sex | N | Minimum | Maximum | Mean | Std.
Deviation |
Median | Mann-
Whitney U test Z value |
p value | |
| Experiment Effect(Post-Pre) Female
BBS Male |
8
7 |
2
1 |
7
9 |
5.63
5.14 |
1.685
2.545 |
5.50
5.00 |
.709 | .478
NS |
|
| Effect(Post-Pre) Female TUG Male | 8
7 |
0
0 |
1
1 |
.50
.29 |
.535
.488 |
.50
.00 |
.816 | .414
NS |
|
| Control | Effect(Post-Pre) Female
BBS Male |
8
7 |
1
0 |
6
6 |
3.38
2.57 |
2.134
2.225 |
3.00
2.00 |
.765 | .444
NS |
| Effect(Post-Pre) Female TUG Male | 8
7 |
0
0 |
1
1 |
.38
.29 |
.518
.488 |
.00
.00 |
.354 | .724
NS |
|
As shown in the table above, the mean values are taken to find out the effect of the gender of the patients on the interventions, in regards to both the outcome tools. The z value in the experimental is 0.709 and p value 0.478 with BBS and z value 0.816 and p value 0.414 with TUG. The z value in the control group is 0.765 and p value 0.444 with BBS and z value0.354 and p value 0.724 with TUG. Thus it shows that the p value is not significant. This means that the study is free from gender bias.
Table 9
Age and the outcome tools.
Correlations
| Group | Spearman’s rho | p | ||
| Experimenta | Age Effect(Post-Pre) BBS
Effect(Post-Pre) TUG |
-.239
-.411 |
.392
.128 |
NS
NS |
| Effect(Post- Effect(Post-Pre) TUG Pre) BBS | .257 | .355 | NS | |
| Control | Age Effect(Post-Pre) BBS
Effect(Post-Pre) TUG |
-.034
.180 |
.905
.520 |
NS
NS |
| Effect(Post- Effect(Post-Pre) TUG Pre) BBS | .366 | .179 | NS | |
The table above correlates the effect of the age of the patients on the outcome tools. The p value in the table indicates that the age does not have any effect on the outcome tools. Thus both the outcome tools are independent from each other and thus the study is not biased.
DISCUSSION
This study was designed to find out and compare the effectiveness of specific balance strategy and conventional balance training in improving balance in multiple sclerosis patients.
Conventional balance training included gentle stretches, coordination exercises, strengthening exercises for lower limbs, controlled mobility exercises and biofeedback mirror. While the specific balance strategy involved various workstations designed to focus on a specific task that addresses aspects required for balance including functional strength, flexibility, balance strategy practice, sensory integration, and added attention demands during function and multi-task practice. The study involved 30 patients with multiple sclerosis, who fulfilled the inclusion criteria. They were then randomly divided into group 1 and group 2. Conventional balance training was applied on group 1 and group 2 received the specific balance strategy. The 45 minutes sessions was given 4 days a week for 3 weeks.
The results showed that there was a significant improvement in the experimental group (group 2) from 30.87 to 36.27 with a mean improvement value of 5.40. The improvement shown here is highly significant with the t value of 8.259 and p value 0.000. This improvement shown was scored with the help of Berg balance scale. While with the timed up and go score which was measured with the help of Wilcoxon Sign Rank test, the z value was 2.449 and the p value 0.014. This shows that the scores were significant with the timed up and go test. This is further supported by D Cattaneo, J Jonsdottir, M Zocchi et al; balance rehabilitation appeared to be a useful tool in reducing the fall rate and improving balance skills in subjects with multiple sclerosis. Exercises in different sensory contexts have an impact in improving dynamic balance 7. Lord SE, DT Wade, P
W Halligan et al; in their study on MS concluded that task oriented approach and facilitation approach helped in improving walking in patients with gait disturbance 36. Romberg A, Virtanen A, Ruutiainen J et al; walking speed improved in this randomized study with the help of set of exercises including strengthening, aerobic training and task oriented approach. The results confirm that exercise is safe for multiple sclerosis patients and should be recommended for those with mild to moderate disability. Tasks related with balance give better results with respect to intervention on strength of lower limbs or aerobic exercises 35. Fulk GD, said that impaired walking ability, balance, and fatigue are common problems for people with multiple sclerosis (MS) and all of the above symptoms could be managed with task oriented, skilled and intensive rehabilitation31.
The results showed that there was an improvement in the conventional group (group 1) as well. The scores showed improvement from 31.40 to 34.40 with a mean improvement value of 3.00. The improvement shown here also is highly significant with the t value of 5.434 and p value 0.000. This improvement shown was scored with the help of Berg balance scale. While with the timed up and go score which was measured with the help of Wilcoxon sign rank test, the z value was 2.236 and the p value 0.025. This shows that the scores were significant with the timed up and go test. Therefore there was a significant improvement with the conventional set of exercises as well. This can be supported by the following studies, Smedal T, Lygren H, Myhr KM et al; indicated that balance and gait can be improved after physiotherapy based on the Bobath concept30. DeBolt L, & McCubbin, J concluded that the home-based resistance program was well tolerated by participants and offered a practical means to improve leg extensor power in a short period of time 34. (Kraft, Alquist, Lateur) 6; used a progressive resistance training
regimen and demonstrated improved muscle strength in upper and lower extremities. Therefore showed improved gait parameters.
In the inter group analysis, both the groups showed improvement in the balance, which was proven by the unpaired t test. The mean difference was 2.40 with a t value of
3.200 and p value of 0.00341 with respect to the berg balance scale. With the time up and go test the mean difference was 0.07, z value 0.371 and p value 0.710. This was proved by the Mann- Whitney U test. These results suggest that specific balance strategy improves balance in the multiple sclerosis patients. The patients even though they showed improvement in their activities of daily living and gait, their gait speed did not show much of an improvement. However they had an efficient gait with reduced frequency of falls. Thus there is a scope for the study to be done on a larger sample size to get a better insight.This is further supported by Kadriye Armutlu, Rana Karabudak, Gulay Nurlu, in their study on multiple sclerosis, concluded that the combination of motor and sensory strategies in balance training is effective in rehabilitation of ataxia in multiple sclerosis 37.
LIMITATIONS OF THE STUDY
- Although the findings were encouraging, the sample size taken was small. Better clinical implications could be possible if further research could establish this further with a larger sample.
- The intervention was shown effective when tested with the berg balance scale, but though the patients demonstrated efficient gait their speed did not show much improvement with the timed up and go test. Further study with a larger sample could help in establishing better results.
RECOMMENDATIONS.
- Patients with multiple sclerosis showed worsening of symptoms especially fatigue in hot and humid climate and post hot water bath. Further scope arises to find out the effect of climate and temperature in their activities of daily living and exercise performance.
- Also further studies with the similar strategy can be done with other types of multiple sclerosis.
CONCLUSION
Results of the study shows that group 2 (experimental group) which received the specific balance strategy & group 1 which received conventional exercise programme have good effect on improving balance in multiple sclerosis patients. But when both the groups were compared, the group which received specific balance strategy gained better improvement in balance than the group received conventional set of exercises
SUMMARY
It was a comparative study where the objective was to compare the effectiveness of specific balance training strategy with conventional balance exercises to improve balance in multiple sclerosis patients. 30 normal individuals were selected randomly from the population and were divided into group 1, conventional and group 2, experimental. Each group consisted of 15 samples.
The subjects were explained about the study procedure. Group 1 received conventional set of balance exercises and group 2 received the specific balance strategy.
Paired and unpaired‘t’ test, Wilcoxon and Mann Whitney test, was used for statistical analysis. Both the groups showed improvement which was statistically highly significant for improvement in the balance. Group 2 which received specific balance strategy showed more improvement than group 1 which received conventional set of exercises.
Therefore the study concludes that specific balance strategy shows significant improvement in balance in patients with multiple sclerosis.
ANNEXURES 1
CONSENT FORM: FOR VOLUNTEERS
I voluntarily accept for the participation in the study entitled “A COMPARATIVE STUDY ON THE EFFECTIVENESS OF SPECIFIC BALANCE STRATEGY VERSUS CONVENTIONAL BALANCE TRAINING TO IMPROVE BALANCE IN MULTIPLE SCLEROSIS PATIENTS- A RANDOMIZED CONTROLLED TRIAL.”
The nature and hazards involved in these studies have been fully explained to me. I understand that I may withdraw from this study at any time.
I consent to the data being collected and stored at the department of physiotherapy and for the data to be used for the research purposes. I understand that I am assured of my anonymity, and that the data will be treated as a confidential document.
I understand that I may also contact the KSHEMA institutional Ethical committee, if I feel I have been unfairly treated.
Date: Signature:
Name:
Witness: Signature: Name:
Investigators statement:
I have carefully explained the nature of the above studies to the subject. Date: Name:
Signature:
ANNEXURE 2
SUBJECT EVALUATION FORM SL No. :
Name: Age: Sex:
Date of assessment:
Referred by:
History: side affected-
Medical history-
Vital signs: respiratory rate- blood pressure- temperature- Examination: Sensory assessment-
Motor assessment- Berg balance scale- Other systems-
Investigation:
Treatment details
| Pre test score | Post test score | |
| Berg balance scale | ||
| Timed up and go test |
Timed, Up, and Go Test (TUG)
The timed “Up & Go” test measures, in seconds, the time taken by an individual to stand up from a standard arm chair (approximate seat height of 46 cm, arm height 65 cm), walk a distance of 3 meters (approximately 10 feet), turn, walk back to the chair, and sit down again. The subject wears his/her regular footwear. If participant’s usually use assistive devices such as canes or walkers, they should use them during the test, but this should be indicated on the data collection form. No physical assistance is given. While setting up the test area, determine a path free from obstruction.
- Place a chair with arms at one end of the path.
- Mark off a 3 m (10 ft.) distance using tape or a cone or other clear marking.
Start the test
- Speak clearly and slowly. Inform participant of sequence and outcome
- “When I say go, you will stand up from the chair, walk to the mark(cone) on the floor, turn around, walk back to the chair and sit down.” “I will be timing you using the stopwatch.” Ask participants to repeat the instructions to make sure they understand.
- Participant starts with their back against the chair, their arms resting on the arm rests, and their walking aid at hand
- Using a cue like “Ready, set, go” might be useful.
- Either a wrist-watch with a second hand or a stop-watch can be used to time the performance.
BERG BALANCE SCALE
Name Date
Location Rater
ITEM DESCRIPTION SCORE (0-4)
- Sitting to standing
- Standing unsupported
- Sitting unsupported
- Standing to sitting
- Transfers
- Standing with eyes closed
- Standing with feet together
- Reaching forward with outstretched arm
- Retrieving object from floor
- Turning to look behind
- Turning 360 degrees
- Placing alternate foot on stool
- Standing with one foot in front
- Standing on one foot
TOTAL
GENERAL INSTRUCTIONS
Please demonstrate each task and/or give instructions as written. When scoring, please record the lowest response category that applies for each item. In most items, the subject is asked to maintain a given position for specific time. Progressively more points are deducted if the time or distance requirements are not met, if the subject’s performance warrants supervision, or if the subject touches an external support or receives assistance from the examiner.
Subjects should understand that they must maintain their balance while attempting the tasks. The choices of which leg to stand on or how far to reach are left to the subject. Poor judgment will adversely influence the performance and the scoring.
Equipment required for testing are a stopwatch or watch with a second hand, and a ruler or other indicator of 2, 5 and 10 inches (5, 12.5 and 25 cm). Chairs used during testing should be of reasonable height. Either a step or a stool (of average step height) may be used for item #12.
- SITTING TO STANDING
INSTRUCTIONS: Please stand up. Try not to use your hands for support. ( ) 4 able to stand without using hands and stabilize independently
( ) 3 able to stand independently using hands
( ) 2 able to stand using hands after several tries ( ) 1 needs minimal aid to stand or to stabilize
( ) 0 needs moderate or maximal assist to stand
- STANDING UNSUPPORTED
INSTRUCTIONS: Please stand for two minutes without holding. ( ) 4 able to stand safely 2 minutes
( ) 3 able to stand 2 minutes with supervision ( ) 2 able to stand 30 seconds unsupported
( ) 1 needs several tries to stand 30 seconds unsupported ( ) 0 unable to stand 30 seconds unassisted
- SITTING WITH BACK UNSUPPORTED BUT FEET SUPPORTED ON FLOOR OR ON A STOOL
INSTRUCTIONS: Please sit with arms folded for 2 minutes. ( ) 4 able to sit safely and securely 2 minutes
( ) 3 able to sit 2 minutes under supervision ( ) 2 able to sit 30 seconds
( ) 1 able to sit 10 seconds
( ) 0 unable to sit without support 10 seconds
- STANDING TO SITTING
INSTRUCTIONS: Please sit down.
( ) 4 sits safely with minimal use of hands ( ) 3 controls descent by using hands
( ) 2 uses back of legs against chair to control descent
( ) 1 sits independently but has uncontrolled descent ( ) 0 needs assistance to sit
- TRANSFERS
INSTRUCTIONS: Arrange chairs(s) for a pivot transfer. Ask subject to transfer one way toward a seat with armrests and one way toward a seat without armrests. You may use two chairs (one with and one without armrests) or a bed and a chair.
( ) 4 able to transfer safely with minor use of hands ( ) 3 able to transfer safely definite need of hands
( ) 2 able to transfer with verbal cueing and/or supervision ( ) 1 needs one person to assist
( ) 0 needs two people to assist or supervise to be safe
- STANDING UNSUPPORTED WITH EYES CLOSED INSTRUCTIONS: Please close your eyes and stand still for 10 seconds. ( ) 4 able to stand 10 seconds safely
( ) 3 able to stand 10 seconds with supervision ( ) 2 able to stand 3 seconds
( ) 1 unable to keep eyes closed 3 seconds but stays steady ( ) 0 needs help to keep from falling
- STANDING UNSUPPORTED WITH FEET TOGETHER
INSTRUCTIONS: Place your feet together and stand without holding.
( ) 4 able to place feet together independently and stand 1 minute safely
( ) 3 able to place feet together independently and stand for 1 minute with supervision ( ) 2 able to place feet together independently and to hold for 30 seconds
( ) 1 needs help to attain position but able to stand 15 seconds feet together
( ) 0 needs help to attain position but unable to stand 15 seconds with feet together.
- REACHING FORWARD WITH OUTSTRETCHED ARM WHILE STANDING
INSTRUCTIONS: Lift arm to 90 degrees. Stretch out your fingers and reach forward as far as you can. (Examiner places a ruler at end of fingertips when arm is at 90 degrees. Fingers should not touch the ruler while reaching forward. The recorded measure is the distance forward that the finger reaches while
the subject is in the most forward lean position. When possible, ask subject to use both arms when reaching to avoid rotation of the trunk.)
( ) 4 can reach forward confidently >25 cm (10 inches) ( ) 3 can reach forward >12.5 cm safely (5 inches)
( ) 2 can reach forward >5 cm safely (2 inches) ( ) 1 reaches forward but needs supervision
( ) 0 loses balance while trying/ requires external support
- PICK UP OBJECT FROM THE FLOOR FROM A STANDING POSITION INSTRUCTIONS: Pick up the shoe/slipper which is placed in front of your feet. ( ) 4 able to pick up slipper safely and easily
( ) 3 able to pick up slipper but needs supervision
( ) 2 unable to pick up but reaches 2-5cm (1-2 inches) from slipper and keep balance independently ( ) 1 unable to pick up and needs supervision while trying
( ) 0 unable to try/needs assist to keep from losing balance or falling
- TURNING TO LOOK BEHIND OVER LEFT AND RIGHT SHOULDERS WHILE STANDING INSTRUCTIONS: Turn to look directly behind you over toward left shoulder. Repeat to the right. Examiner may pick an object to look at directly behind the subject to encourage a better twist turn.
( ) 4 looks behind from both sides and weight shifts well
( ) 3 looks behind one side only other side shows less weight shift ( ) 2 turn sideways only but maintain balance
( ) 1 needs supervision when turning
( ) 0 needs assist to keep from losing balance or falling
- TURN 360 DEGREES
INSTRUCTIONS: Turn completely around in a full circle. Pause. Then turn a full circle in the other direction.
( ) 4 able to turn 360 degrees safely in 4 seconds or less
( ) 3 able to turn 360 degrees safely one side only in 4 seconds or less ( ) 2 able to turn 360 degrees safely but slowly
( ) 1 needs close supervision or verbal cueing ( ) 0 needs assistance while turning
- PLACING ALTERNATE FOOT ON STEP OR STOOL WHILE STANDING UNSUPPORTED
INSTRUCTIONS: Place each foot alternately on the step/stool. Continue until each foot has touched the step/stool four times.
( ) 4 able to stand independently and safely and complete 8 steps in 20 seconds ( ) 3 able to stand independently and complete 8 steps >20 seconds
( ) 2 able to complete 4 steps without aid with supervision ( ) 1 able to complete >2 steps needs minimal assist
( ) 0 needs assistance to keep from falling/unable to try
- STANDING UNSUPPORTED ONE FOOT IN FRONT
INSTRUCTIONS: (DEMONSTRATE TO SUBJECT)
Place one foot directly in front of the other. If you feel that you cannot place your foot directly in front, try to step far enough ahead that the heel of your forward foot is ahead of the toes of the other foot. (To score 3 points, the length of the step should exceed the length of the other foot and the width of the stance should approximate the subject’s normal stride width)
( ) 4 able to place foot tandem independently and hold 30 seconds
( ) 3 able to place foot ahead of other independently and hold 30 seconds ( ) 2 able to take small step independently and hold 30 seconds
( ) 1 needs help to step but can hold 15 seconds ( ) 0 loses balance while stepping or standing
- STANDING ON ONE LEG
INSTRUCTIONS: Stand on one leg as long as you can without holding. ( ) 4 able to lift leg independently and hold >10 seconds
( ) 3 able to lift leg independently and hold 5-10 seconds
( ) 2 able to lift leg independently and hold = or >3 seconds
( ) 1 tries to lift leg unable to hold 3 seconds but remains standing independently ( ) 0 unable to try or needs assist to prevent fall
( ) TOTAL SCORE (Maximum = 56)
REFERENCES
- Susan B O’ Sullivan. Physical rehabilitation assessment and treatment; Multiple sclerosis. 4th edition, pg 715 Jaypee Brothers; 2001.
- Bansil S, Singhal BS, Ahuja GK, Ladiwala U, Behari M, Friede R, Cook SD. Comparison between multiple sclerosis in India and the United States: a case- control study. Journal Neurology 1996 Feb; 46(2):385-87.
- Singhal BS. Multiple sclerosis–Indian experience. Ann Acad Med Singapore.1985 Jan; 14(1):32-6.
- John Walton. Brain’s diseases of the nervous system, Chapter 10. Multiple sclerosis.10th edition, 1993, pg 366, Oxford university press.
- Aronson K, Goldenberg E, Cleghorn G: socio-demographic characteristics and health status of persons with multiple sclerosis and their care givers, MS Management 3(1):5-15, 1996.
- Darcy A Umphred, Debra I, Frenkel. Neurological rehabilitation, chapter 22, multiple sclerosis, 5th edition, 2007, pg 709, Mosby Elsevier publication.
- D Cattaneo, J Jonsdottir, M Zocchi and A Regola LaRice. Effects of balance exercises on people with multiple sclerosis: a pilot study, Clinical Rehabilitation 2007; 21: 771–781.
- Jennifer C Nitz, Nancy Low Choy. “The efficacy of a specific balance strategy training programme for preventing falls among older people: a pilot randomized controlled trail.” Age and aging 2004;33:52-58.DOI:10.1093/ageing/afh028.
- Cameron MH, Horak FB, Herndon RR, and Bourdette D. “Imbalance in multiple sclerosis: a result of slowed spinal somatosensory conduction.”J Neurol 2008 mar; 255 suppl 1:75-83.PMID18570015
- Kesselring J, Beer S “Symptomatic therapy and neurorehabilitation in multiple sclerosis”Lancet neurology 2005: 4(10):643-52.PMID 16168933
- Woorlacott MA. “Systems contributing to balance disorders in older adults.” J Gerontol Med Sci 2000; 55A:M424-8.
- Frzovic D, Morris ME, and Vowels L. “Clinical tests of standing balance: performance of persons with multiple sclerosis.” Arch phys med rehabil 2000; 81:215-21.
- Williams NP, Roland PS, Yellin W. “Vestibular evaluation in patients with early multiple sclerosis.”Am J otol 1997; 18:93-100?
- Daley ML, Swank RL. “Quantitative posturography use in multiple sclerosis.”IEEE trans biomed eng 1981;28:668-71
- Cattaneo D,DL Nuzzo C, Fascia T, Macalli M, Pisoni I, Cardini R. “Risks of falls in subjects with multiple sclerosis.”Arch phys med rehabil 2002; 83:864-67.
- Joel A DeLisa, James A Sliwa and Bruce A Cohen. Rehabilitation medicine Principles and Practice. Multiple sclerosis, chap 50, pg 1241, 3rd edition, Lippincott Raven.
- McDonald WI, Compston A, Edan G, et al. “Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis”. Ann. Neurol. July 2001; 50 (1): 121–7. PMID 11456302.
- Rosati G. “The prevalence of multiple sclerosis in the world: an update”. Neurol.
Sci. April 2001; 22 (2): 117–39. PMID 11603614.
- Kenneth n Anderson and Lois E Anderson. Mosby’s Pocket Dictionary of Medicine and Allied Health., 1st edition, 1993
- Compston DA: Mc alpine’s Multiple Sclerosis, 3rd edition, 1998, Churchill Livingstone.
- Zaffaroni M, Ghezzi A: the prognostic value of age, gender, pregnancy and endocrine factors in multiple sclerosis. Neurol sci 21:s857-s860, 2000.
- Paty DW, Ebers GC: Multiple sclerosis, Philadelphia, 1998.
- Kraft GH, Freal JE, Coreyll JK, et al: ms: early prognostic guidelines, arch phys med rehabil 62(2):54-58, 1981.
- Davis, F. A., Bergen, D., Schauf, C., et al movement phosphenes in optic neuritis: a new clinical sign. J Neurology July 1976, 26, 1100.
- Honan, W. P., Heron, J. R., Foster, D. H and Snelgar R S. Paradoxical effects of temperature in MS. J neurol neurosurg.psychiat. 1987, 50, 1160.
- Freeman JA, et al. Outcome measures to quantify the effects of physical therapy for people with multiple sclerosis. Neurology Report 2002, 26(3):139–144.
- Stolp-Smith, K. Et al: Management of impairment, disability, due to multiple sclerosis mayo clinic proc 72:1184, 1997.
- Kasser, Susan L, Rose, Debra J, Clark, Sean. Balance training for adults with multiple sclerosis: Multiple case studies. Neurology Report, Mar 1999.
- Soyuer F, Mirza M, Erkorkmaz U. Balance performance in three forms of multiple sclerosis. Neurol Res. 2006 Jul; 28(5):555-62.
- Smedal T, Lygren H, Myhr KM, Moe-Nilssen R, Gjelsvik B, Gjelsvik O, Strand LI. Balance and gait improved in patients with MS after physiotherapy based on the Bobath concept. Physiother Res Int. 2007 Mar; 12(1):52.
- Fulk GD. Locomotor training and virtual reality-based balance training for an individual with multiple sclerosis: a case report. J Neurol Phys Ther. 2005 Mar; 29(1):34-42.
- Steinberg M, Cartwright C, Peel N, Williams G. A sustainable programme to prevent falls and near falls in community dwelling older people: results of a randomised trial. J Epidemiol Commun Health 2002; 54: 227–32.
- Allen A, Simpson JM. A primary care based fall prevention programme.
Physiother theory Practice 1999; 15: 121–33.
- DeBolt L., & Mc Cubbin, J. (2004). The effects of home-based resistance exercise on balance, power, and mobility in adults with Multiple Sclerosis. Arch Phys Med Rehabil, 85, 290-297.
- Romberg A, Virtanen A, Ruutiainen J et al. “Effects of a 6 month exercise program on patients with multiple sclerosis: a randomized controlled study.” Neurology 2004; 63:2034-38.
- S E Lord, D T Wade, P W Halligan. A comparison of two physiotherapy treatment approaches to improve walking in multiple sclerosis: a pilot randomized controlled study. Clinical Rehabilitation, Vol. 12, No. 6, 477-486 (1998)
- Kadriye Armutlu Rana Karabudak Gülay Nurlu. Physiotherapy Approaches in the Treatment of Ataxic Multiple Sclerosis: A Pilot Study. Neurorehabilitation and Neural Repair, Vol. 15, No. 3, 203-211 (2001)DOI: 10.1177/154596830101500308.
- White LJ, Dressendorfer RH, Exercise and Multiple sclerosis, sports med 2004;34(15):1077-100.
- Cattaneo D, Jonsdottir J, Repetti S. Reliability of four scales on balance disorders in persons with multiple sclerosis, Disabil rehab. 2007 dec30; 29(24):1920-5. Epub 2007 Apr26.
- Riddle DL, Stratford PW. Interpreting validity indexes for diagnostic tests: an illustration using the Berg balance test. Phys Ther 1999; 79: 939–48.
- Cattaneo D, Regola A, Meotti M. Validity of six balance disorders scales in persons with multiple sclerosis. Disabil rehabil 2006 jun30; 28(12):789-95.
- Podsiadlo D, Richardson S. The timed ‘up and go’: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39: 142–8.
- Martin CL, Phillips BA, Kilpatrick TJ, Butzkueven H, Tubridy N, McDonald E, Galea MP. Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Mult sclera 2006 Oct; 12(5):620-8.