Comparison between the effects of core exercises with Mckenzie method versus core exercises with Myofascial release Technique in stage – 2 of lumbar disc prolapse – Dr. Manash Kanti Chakraborty,
Comparison between the effects of core exercises with Mckenzie method versus core exercises with Myofascial release Technique in stage – 2 of lumbar disc prolapse
Dr. Manash Kanti Chakraborty, MPT Ortho, Deepika Tanwar, MPT Ortho
ABSTRACT
STUDY OBJECTIVES: Comparison between the effects of core exercises with Mckenzie method versus core exercises with Myofascial release Technique in stage – 2 of lumbar disc prolapse.
DESIGN: Pre-test and post-test two group comperative study design. PARTICIPANTS: Thirty subjects aged 30-50 years with clinically diagnosed as stage -2 lumbar disc prolapse were selected under randomized sampling technique and assigned in to two groups with 15 subjects each, one group received core exercises with Mckenzie method and other group core exercises with Myofascial release Technique for a period of 12 weeks.
OUTCOME MEASURES: Visual Analogue Scale (VAS) and Oswestry Disability Questionnaire (ODQ)
RESULT: Patients in core exercises with Myofascial release group shows significantly better than core exercises with Mckenzie method group.
KEY POINT: Core Exercises, Mckenzie method, Myofascial release technique, stage – 2 of lumbar disc prolapse.
INTRODUCTION
A prolapsed lumbar disc is a spine condition that can cause lower back pain, numbness, tingling and muscle weakness in the lower body.it can happen to people of all ages, but becomes more common after the age of 35.
Herniated lumbar disc material (nucleus pulposus or annulus fibrosus) beyond the intervertebral disc space. The highest prevalence is among people aged 30-50 years, with a male to female ratio of 2:1. In people aged 25-55 year, about 95% of herniated discs occur at the lower lumbar spine (l4/5andl5/s1 levels); disc herniation abovet his level is more common in people aged over 55 years.
A prolapsed lumbar disc can occur anywhere in the lumbar region of the spine, specially the vertebrae at the base the disc between these relatively flexible lumbar vertebrae prone to prolapse because the lower back support much of the body’s weight.
As the body ages the discs between our vertebrae begin to lose their elasticity and their ability to bounce back from everyday movement .this creates pressure which pushes the soft inner disc against the fibrous outer layer. Eventually the disc wall can tear and inner material pushes into the spinal column, resulting in a prolapsed disc.
International surveys of low back pain reported that one month prevalence was 19 – 43 % and point prevalence was 15 – 30 %.
The estimated worldwide life time prevalence of low back pain varies from 50 – 84 % .
Experts estimate up to 80% of population will experience back pain at some time of their lives. Worldwide, years lived with disability caused by low back pain have increased by 54
% between 1990 and 2015.
In India over all the prevalence of low back pain found to be 42%. The majority of women (60.9%) with low back pain experienced moderate disability . prevalence of low back pain among women was comparatively more then other studies in India.
There are many back pain myths
- Myth: always sit up straight
Fact: slouching is bad, but sitting up too straight and still for long periods can also be a strain on back.
- Myth : don’t lift heavy things.
Fact : it’s not necessarily how much you lift it’s how you do it .
- Myths : bed rest is the best cure.
Fact : yes, resting can help a recent injury or strain that causes back pain, but a day or two in bed can actually make it worse.
- Myth : exercise is bad for back pain.
Fact : regular exercise prevent back pain.
- Myth : firmer mattresses are better. Fact : medium firm mattress hurt less.
TheMcKenziemethodisaclassificationsystemandaclassificationbasedtreatmentfor patients withlowbackpain. Aacronymfor the Mc Kenziemethodismechanical diagnosis and therapy (MDT) the M c Kenzie method was developed in 1981 byrobin Mc. Kenzie a physical therapist from new Zealand .
Mckenzie exercise are designed to reposition any displaced intervertebral disc. This is initially done by using gravity to draw the disc back into the spine and then actively consolidate the effect of gravity. To facilitate disc movement, when performing the exercise and maintain relaxed and even breathing for the duration of exercise.
The Mckenzie method also referred to as mechanical diagram and therapy is a method of assessing and treating spinal back join and related extremity pain most commonly through the use of specific repeated movements and appropriate prevention measures. The method puts an emphasis on self-core after initial clinical visits it uses primarily self-treatment strategies and minimizes manual therapy procedure with the Mc.kenzie trained therapist supporting the patient with passive procedures only if an individual self- treatment program is not fully effective.
The Mckenzie method also referred to as mechanical diagnosis and therapy is a method of assessing and treating spinal back pain and related extremity pain most commonly through the use of specific repeated movements and appropriate prevention measures.
Centralization – centralization occurs when pain symptoms off-centered from the mid-line of the spine often diagnosed as sciatica, migrate towards the centre of mid-line of the spine this migration of pain symptoms to the centre of lower back is a sign of progress in the Mckenzie method. The most common directional preference that result in centralization is extension of the back.
Classification – there are three primary classification that results from the assessment portion of the Mckenzie method comprehensive approach ; postural syndrome, dysfunction syndrome and derangement syndrome.
Derangement syndrome – the most common treatment classification defined by pain that is experienced due to a disturbance in the joint area resulting in diminished movement in certain directions.
Dysfunction syndrome – this type of pain is categorized by mechanical impairments and deformities of impaired tissue within the body.
Postural syndrome – this type of pain is the result of postural deformation position such as slouching are the cause of postural syndrome.
The McKenzie method exists of 3 steps
- Evaluation
- Treatment
- Prevention
The evaluation is received using repeated movements and sustained positions, with the aim to elicit a pattern of pain responses called centralization .The symptoms of lower limb and lower back are classified into three sub groups: derangement syndrome, dysfunction syndrome and postural syndrome.
The prevention step consist of encouraging the patient to exercise regularly and self-care. The choice of exercises in the McKenzie method is based upon the direction (flexion,
extension or lateral shift of the spine)
The McKenzie method educates patients regarding movement and position strategies can reduce pain.
Principle –
- Kyphotic antalgic management: extension principle
- Acutec or on a lantalgic management: lateral flexion– then– extension principle
- Acute lordotic antalgic management: flexion principle.
Core exercises are a crucial part of any exercise regimen. These exercises strengthen the body, particularly the pelvis hip and lower back areas.
Some examples of this type of exercise include crunches, reverse crunches, ball crunches, and oblique
Crossing over crunches air bicycling plank, butt lifts, back extension with ball and many more.
These exercises work on the deep abdominal muscles, strengthen abs and flatten them, core exercises also make the lower back stronger and healthier.
Doing core exercises stimulates a particular area in the brain called the cerebellum that links to body parts for coordination, spatial awareness.
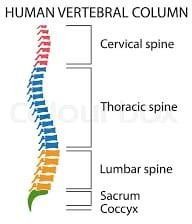
Figure No.1
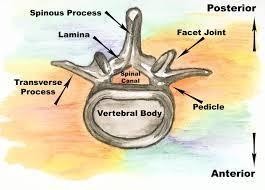
Figure No.2
Mckenzie exercises may be effective in decreasing symptoms, specially leg pain.
Mckenzie exercises centralize back pain, moving it from the leg to the lower back with daily exercises that works to relive acute or chronic pain.
Core exercises support lower back in herniated disc. Core exercises work on lower abdominal muscles.
Core exercises cause flexibility of Spine, give power to muscles provide balance and stability of lower back decrease lower pain and injury.
Core stability is the term used to describe the muscular control required to maintain functional stability around the lumber spine and to prevent lower back pain.
The “core” is often mistaken for the visible abdominal muscles the rectus abdomens, the “abs”, however, the muscles involved can be described as a muscular box and include abdominals in the front (rectus abdominus , transverse abdominus , multifedus, internal oblique) paraspinals and gluteals in the back the diaphragm at the top and the peluic floor on the bottom.
Myofascial release Technique(MFR):
Myofascial release is an alternative medicine therapy that claims to treat skeletal muscle immobility and pain by relaxing contracted muscles, improving blood and lymphatic circulation , and stimulating the stretch reflex in muscles.
The approach was promulgated as an alternative medicine concept by Andrew Toylor still, inventor of osteopathy. The exact phrase “ myofascial release” was coined in the 1960s by Robert ward, an osteopath who studied with Ida Rolf, the originator of rolfing word , along with physical therapist Johan Barnes, are considered the two primary founders of Myofascial release.
Step I: Getting Ready
Step II: Thelengthening processes Step III: Completion
Step IV: Postural integration
Myofascial release is a system of diagnosis and treatment first described by Andrew Taylor still and his early students, which engages continual palpatory feedback to achieve release of myofacial tissues.
Myofascial release techniques have been anecdotally reported as being effective in reliving restrictions and increasing range of motion. Direct MFR techniques engage the restrictive barrier and the tissue is then loaded with a constant force until tissue release/relaxation occurs.
Indirect MRF involves gliding the dysfunctional tissues along the path of least resistance
(away from the barrier) until free movement is achieved.
The goals of myofascial treatment include relaxation of contracted muscles increased circulation to an area of ischemia increase venous and lymphatic drainage and the stimulation of stretch reflexes in hypotonic muscle.
NEED OF THE STUDY
The results of the study may help the physiotherapists to identify and use the appropriate methods in the treatment of stage-2 lumbar disc prolapse patients. This study can also help the physiotherapists in understanding the relation between the different parameters considered for the study under such as VAS (Visual analogue Scale), MMT (Manual muscle Testing), spinal ranges. The study provides an information, that how the study will contribute and who will benefit for it. It includes an explanation of the study’s importance as well as its benefits. By evaluating the results of the study, the physiotherapist able to identify the positive outcomes. The study can help the physiotherapist what impact will these treatment have upon reducing the patient’s problem and promoting health.
With the Mckenzie approach, physical therapy and exercise used to extend the spine can help “centralize” the patient and pain by moving it away from the extremities (leg or arm) to the back.
The long term goal of Mckenzie method is to teach patients suffering from back pain how to treat themselves and manage pain throughout their lives using exercise and other strategies.
Whereas strong core may actually help prevent back pain by making less prone to back injuries and proper spinal alignment. Strengthening core muscles may also help improve back pain.
The focused manual pressure and stretching used in myofascial release therapy loosen up restricted movement leading to reduced pain.
The core exercises with Mckenzie method and core exercises with MFR technique are used in this study to treat the patients and compare the effects of both techniques, because of its effectiveness, easy to understand by the patients, less time consuming and cost effective. Seong Hun Yu, Yong Hyeon Sim, and Hyun Jin kim study the effects of abdominal drawing in exercise and myofascial release on pain flexibility and balance of elderly females who complained of low back pain.
The abdominal drawing in exercise group show significant difference in pain & balance and myofascial release group show significant deference in pain & flexibility after exercise. Macey Berube, BS, in his case report found Mckenzie exercise with core strengthening shows improvement in pain & activity levels motion strength and tenderness.
AIMS OF THE STUDY
To evaluate the comparison of core exercises with McKenzie method in stage-2 lumbar disc prolapse patients. To find the effects of core exercises with Myofascial release Technique in stage- 2 lumbar disc prolapse patients. To compare between the effects of core exercises with Mckenzie method versus core exercises with Myofascial release Technique in stage – 2 of lumbar disc prolapse.
OBJECTIVE OF STUDY
- To evaluate the effects of different exercises
- To compare between the effects of different exercises
- To find out new facts if any at any stage
- To find out the limitations and recommendations
- To verify and test important facts
- To find solution to problem
HYPOTHESIS
Alternate hypothesis:
There is significant difference between the effect of core exercises with McKenzie method and the effect of core exercises with MFR in stage-2 lumbar disc prolapse patients
Null hypothesis:
There is no significant difference between the effect of core exercises and core exercises with Mckenzie method in patient with stage- 2 lumbar disc prolapse.
MATERIALS
Materials used:
- Couch : used for treatment and comfortable position of the patients
- Timer : used to note the treatment time
- Pillows : used to support body parts
- Goniometer: used to measure range of motion of joints
- Paper
- Pencils
- Duly signed Consent forms
OUTCOME MEASURE
- VISUAL ANALOGUE SCALE (VAS)
OSWESTRY DISABILITY QUESTIONNAIRE (ODQ)
METHODOLOGY
STUDY DESIGN
This study design involving the comparative analysis of two groups treated with core exercises with McKenzie method and core exercises with Myofascial release Technique respectively and assessed by VAS (Visual analogue Scale), MMT (Manual muscle Testing) ,spinal ranges.
SAMPLE SIZE:
Fourty subject with stage-2 lumbar disc prolapse aged between 30-50 years were selected according to convenience (purposive) sampling based on the selection criteria.
These subject were then randomly assigned into two groups of twenty subjects each namely experimental group A and experimental group B.
All the participants took part in the experiment on a voluntary basis after signing a consent from and a demographic data was collected from each subject. The purpose of the study was explained to all the subjects.
SAMPLING METHOD: Experimental method STUDY CENTRE: College Opd Dabok INCLUSION CRITERIA:
- Patients clinically diagnosed as stage -2 lumbar disc prolapse.
- Age group from 30-50 years.
EXCLUSION CRITERIA:
- Patients with grade 3, 4 lumbar disc prolapse.
- Age less than 30 and more than 50 years. History of any recent spine surgery.
- History of any spinal diseases.
STUDY DURATION:
- Total duration of study: 12 weeks
- Sessions:1 Session per day
- Duration of sesson:15 to 30 minutes
- Days per week:5 days a week
MEASUREMENT TOOLS:
- Visual analogue scale(VAS)
- Manual muscle testing (MMT)
- Spinal ranges
- Oswestry disability questionnaire(ODQ)
Visual analogue scale(VAS): It was used for pain assessment where by pain was rated from 0
– 10 in which the ‘0’ represented no pain and 10 represented maximum pain tolerance subject were indicated the best number for their pain.
Manual muscle testing (MMT): Manual muscle tests are performed daily by Physiotherapists not only is it used to help predict a patients ability to function it provides a reference with which to document progress.
Grades of MMT-
- none – no visible or palpable contraction
- trace – visible or palpable contraction with no motion. 2 poor – full ROM gravity eliminated
3 fair – full ROM against gravity
good – full ROM against gravity, moderate resistance. 5 normal – full ROM against gravity, maximal resistance .
Spinal ranges – the lumbar spine commonly known as the low back is also tested during range of motion exams the lumbar spine has five vertebrae and connects the spine to the pelvis normal lumbar ranges of motion include 60 degree of flexion 25 degree of extension and 25 degree of lateral or side bending .
Oswestry disability questionnaire (ODQ) : ODQ was completed to assesses percentages of functional disability in patients with lumbar disc prolapse this questionnaire is a gold standard tool indicate ability of patients with lumbar disc prolapse . it consist of 10 section and each of the section includes 6 rates from 0-5. The first section of this questionnaire rates pain and the other section assesses activities of daily living total score of questionnaire was recorded as percentage.
PROCEDURE
40 subject clinically diagnosed as stage-2 lumbar disc prolapse was selected according to inclusion and exclusion criteria and divided randomly into two groups ; namely experimental group A and experimental group B, consisting of 20 subject each.
A brief explanation about the treatment session will explained to all the subjects. The treatment duration for both the group will given as listed below:
Duration per session: 15-30 minutes /session No. of session per day : 1session /day No. of days per week : 5 days a week Duration of the study : 3 months
The visual analogue scale, manual muscle testing , spinal ranges and oswestry disability questionnaire were noted before and at the end of 4th week of treatment group A will treated with core exercises and Mckenzie method group B received core exercises with myofascial technique.
Group A (core exercises with Mckenzie methods): the subject will in a comfortable position support your lower back by sitting upright in a firm chair place feet firmly on floor. Tighten abdominal muscles and bring belly button toward the back of the chair. Hold this tension for 10 seconds.
Bird dog – start on all four limbs and extend the left leg behind you while extending the right arm in front with your thumb up. Compress your abdominal muscles and hold for 10-20 seconds then repeat on the opposite side.
Plank – plank is basically the position in when you are at the top of a push-up. Hold it as long as possible, drawing in your stomach and compressing your lower abs.
Abdominal draw – in supine position drawing the lower abdomen in and then drawing up the pelvic floor muscle so that it contract together with their lower abdomen.
McKenzie exercises fall into 2 categories with opposite movement extension and flexion. Extension and flexion exercises involve moving the spine in opposite directions. Extension exercises by moving spine backward, which is spinal extension. Lie on your abdomen and work up to raising your head and chest off the floor to prop yourself up onto your elbow flexion exercises involve bending the spine forward, in the opposite direction as spinal extension . flexion exercises can be perform by seated standing or lying on back . bringing knees to your chest while lying down is an example of a lying flexion exercise. (Reference No.14)
Group B core exercises with MFR (Myofascial release technique): core exercises are mention above with MFR (Myofascial release technique)
- Land on the surface of the body with the appropriate “tool” (knuckles, or forearm tc)
- Sink in to the soft tissue.
- Contact the first barrier/restricted layer.
- Put in a “line of tension”.
- Engage the fascia by taking up the slack in the tissues.
- Finally move or drag the fascia across the surface while staying it touch with the underlying layers.
- Exit gracefully.
- Data collection-
All the data was collected with outcome measure and kept safely for statistical analysis.
- Statistical test-
An appropriate statistical tests will be applied to the data for analysis.
- Limitation-
Will be able to present only after the detail study has been carried out.

Figure No.3 McKenzie extension exercise

Figure No.4 McKenzie extension exercise

Figure No.5 Bridging exercise

Figure No.6 Plank variation

Figure No.7 Myofascial release technique

Figure No.8 Myofascial release technique

Figure No.9 Myofascial release technique

Figure No.10 Myofascial release technique
DATA ANALYSIS
Pre-test and post test data within group and between group well be analyses by paired and un paired ‘t’ test.
The differences between pre test and post test values were found the mean deference VAS of A compared with group B and the actual pattern of variation were observed.
With the ‘t’ value from the pre test and post test the accurate level of significance was analyses and interpreted.
An alpha level of p < 0.05 was the level of significant for the test Arithmetic mean: –
X̅ =∑x∕N Where,
X = Arithmetic mean
∑x= sum of all variables
N= total number of variables Standard deviation (s.d)
s.d= √(X-X̅ )2 /√N where,
x̅ = mean of scores
X = sum of all variable N = total no of variables (X-X̅ ) = deviation
Paired ‘t’ Test within group:
The paired ‘t’ test was used to find out the significance within the same group with the values of parameters considered for the study.
The formula to find the value of “t” using paired ‘t’ test:
t= [M1-M2]/SEMd
Where,
M1= Mean 1
M2= Mean 2
SEMd= Standard error of mean difference SEMd= √SEM12 + SEM22 – 2r SEM1 SEM2
r=correlation between GROUP A and GROUP B df=N-1
UNPAIRED ‘t’ TEST BETWEEN GROUP:
The ‘t’ test was used to find out the significance between the groups and it gives the variable information regarding this study.
The formula to find the value of ‘t’ using unpaired ‘t’ test for GROUP A via GROUP B: t=[M1-M2]/SEMd
where,
M1= Mean 1 M2 = mean 2
SEMd=Standard error of mean difference SEMd =√SEM12 +SEM22
SEM1 = Ꝺ1/√N1 SEM2= Ꝺ2/√N2
Demographic presentation of data in group
40 subject of age group 30-50 years were randomly selected according to inclusion and exclusion criteria and divided into two group with 20 subjects in each group. group A had a mean age of 38.6 years and group B had a mean age of 41.9 the demographic data of both the groups has been presented in table 5.1.
Table 5.1 demographic presentation of data in graph:
| Age in year | ||||
| Group | Number | Mean | S.D | |
| Group A | 20 | 38.6 | 6.40 | |
| Group B | 20 | 41.9 | 6.17 | |
| Total | 40 | 40.25 | 6.506 | |
Demographic presentation of data in group
Graph
45
41.9
40
38.6
35
30
25
20
15
10
6.4
6.17
5
0
Group A
Group B
Group A Group B
Figure:5.1
Analysis of pre-test and port-test value of pain using visual analogue scale (VAS) for significance within Group A:
The pain score due to lumber disc prolapse of each subject in group A was assessed by using visual analogue scale (V.A.S) before the start of the treatment as pre-test values and at the end of 3rd month as post-test values the data has been presented in table and depicted in figure 5.2
Table:5.2 analysis of pre-test and post-test values of pain scores using visual analogue scale (VAS)
For significance within group A.
| Mean | N | S.D | Std Error
Mean |
Mean Deference | T | P | Significance | |
| Pre-test | 4.15 | 20 | 1.24 | 0.27 | ||||
| VAS | 3.7 | 13.70 | 0.00002 | significant | ||||
| Post-test | 0.45 | 20 | 0.49 | 0.11 |
Interpretation – the above table shows the mean of pre-test and post-test VAS values were 4.15 and 0.45 respectively. the mean improvement in pain scale of groups was 3.7 the ‘t’ value 13.70 and ‘p’ values 0.00002 for pain scores using VAS within group A analysis.
When compared to table value . the above ‘P’ value is lesser at p < 0.05 which is significant it indicate that group A treated with core exercises with Mckenzie method had less significant in pain intensity.
Analysis of pre-test and post test values of pain scores using visual analogue scale (VAS) for significance with group B:
The pain sore due to lumber disc prolapse of each subject in group B was assessed by using visual analogue scale (VAS) before the start of the treatment as pre-test values and at the end of 3rd month as post test value the data has been presented in table 5.3 and depicted in figure 5.3
Table 5.3 analysis of pre-test and post test values of pain scores using visual analogue scale (VAS) for significant within group B.
| Mean | N | S.D | Std.Error
Of Mean |
Mean
Difference |
T | P | Significance | |
| Pre-test | 3.55 | 20 | 1.68 | 0.375 | ||||
| VAS | 3.15 | 7.5 | 0.00003 | significant | ||||
| Post-test | 0.4 | 10 | 0.48 | 0.107 |
Interpretation – the above table shows the mean of pre-test and post-test VAS values were 3.55 and 0.4 respectively the mean improvement in pain score group b was 3.15 the ‘t’ value 7.5 and ‘P’ value 0.00003 for pain score using VAS within group B analysis when compared to table value , the above ‘p’ value is lesser at p<0.05 which is significant. It indicates that group B treated with core exercise with MFR had significant improvement effect in pain intensity .
Fig 5.2 . analysis of pre-test and post-test values of pain scores using visual analogue scale (VAS) for significant within group A.
Chart Title
4.5
4.15
4
3.5
3
2.5
2
1.5
1.24
1
0.45 0.49
0.5
0
pre-test
post-test
Series 1 Series 2
Figure 5.3 analysis of pre-test and post-test values of pain scores using visual analogue scale (VAS) for significant within Group B
Chart Title
4
3.55
3.5
3
2.5
2
1.5
1
0.5
0
Pre-test
Post-test
Series 1 Series 2
| 1.68 | 0.4 0.48 | |||||
Analysis of Pre-test values of pain scores using VAS of lumber disc proper between group
The pain score of lumber disc prolapse of each subject in group A and group B were assessed by using visual analogue scale (VAS) before the start of the treatment as pre-test values .the values of group A & group B were compared between groups for significance of treatment the data has been presented in table 5.4.
Tables 5.4 Analysis of pre-test values of pain scores using VAS for significance between group.
| Group | Mean | N | S.D | Std Error
Of Mean |
Mean
Deference |
T | P | Significance | |
| VAS | A | 4.15 | 20 | 1.24 | 0.27 | ||||
| 0.60 | 3.7 | 0.000062 | significant | ||||||
| Pre-test | B | 3.55 | 20 | 1.68 | 0.375 |
Interpretation
The above table shows the mean of free test values of pain scores were 4.15 and 3.55 in group A and group B respectively .the mean deference in pain scores between group were 0.60 . the ‘t’ value 3.7 and ‘P’ value 0.00062 for pain scores of lumbar disc prolapse between group a and group B analysis when compared the table value the above ‘P’ value is lesser at p < 0.05 which is significant ,
Analysis of post-test values of pain scores using VAS of lumbar disc prolapse between groups.
The pain scores of lumbar disc prolapse of each subject in group a and group b were assist by using VAS at the end of third month as post-test values. The value of group a and group b were compared between group for significance of treatments .
Analysis of post test values of pain scores using VAS for significance between groups
| Group | Mean | N | S.D | Std.Error Mean | Mean Deff. | T | P | Significance | |
| VAS
Post- Test |
A | 0.45 | 20 | 0.49 | 0.11 | ||||
| 0.05 | 0.32
2 |
0.016 | Non-
Significant |
||||||
| B | 0.4 | 20 | 0.48 | 0.105 |
Interpretation the above table show the post-test value for group a and group b of mean 0.45 and 0.4 respectively and ‘t’ value 0.322 for pain score using VAS between groups. When compared to table value, the above p value is 0.016 at p < 0.05, which is greater it indicates that technique were effective in lumber disc prolapse but the group A treated with core exercises with Mckenzie method has less effect then group B treated with core exercise MFR in subjects
Mean improvement in all the parameter between group A and group B
The pain score of each subject in group A and group B were assessed by using VAS before the start of the treatment and at the end of third month the mean improvement in pain score were compared between both the group.
| Group | Mean | N | S.D | Std Error
Of Mean |
Mean
Deference |
T | P | Significance | |
| VAS | A | 4.15 | 20 | 1.24 | 0.27 | ||||
| 0.60 | 3.7 | 0.000062 | significant | ||||||
| Pre-test | B | 3.55 | 20 | 1.68 | 0.375 |
Interpretation
The above table shows the mean of free test values of pain scores were 4.15 and 3.55 in group A and group B respectively .the mean deference in pain scores between group were 0.60 . the ‘t’ value 3.7 and ‘P’ value 0.00062 for pain scores of lumbar disc prolapse between group a and group B analysis when compared the table value the above ‘P’ value is lesser at p < 0.05 which is significant ,
Analysis of post-test values of pain scores using VAS of lumbar disc prolapse between groups.
The pain scores of lumbar disc prolapse of each subject in group a and group b were assist by using VAS at the end of third month as post-test values. The value of group a and group b were compared between group for significance of treatments .
Analysis of post test values of pain scores using VAS for significance between groups
| Group | Mean | N | S.D | Std.Error Mean | Mean Deff. | T | P | Significance | |
| VAS
Post- Test |
A | 0.45 | 20 | 0.49 | 0.11 | ||||
| 0.05 | 0.32
2 |
0.016 | Non-
Significant |
||||||
| B | 0.4 | 20 | 0.48 | 0.105 |
Interpretation the above table show the post-test value for group a and group b of mean 0.45 and 0.4 respectively and ‘t’ value 0.322 for pain score using VAS between groups. When compared to table value, the above p value is 0.016 at p < 0.05, which is greater it indicates that technique were effective in lumber disc prolapse but the group A treated with core exercises with Mckenzie method has less effect then group B treated with core exercise MFR in subjects
Mean improvement in all the parameter between group A and group B
The pain score of each subject in group A and group B were assessed by using VAS before the start of the treatment and at the end of third month the mean improvement in pain score were compared between both the group.
| Group | No | Age In Years | |
| Mean | S.D | ||
| Group A | 20 | 38.6 | 6.40 |
| Group B | 20 | 41.9 | 6.17 |
| Total | 40 | 40.25 | 6.506 |
Within group:
Group A
| Mean | N | S.D | Std.Error
Mean |
Mean
Difference |
T | P | |
| Pre-Test | 4.15 | 20 | 1.24 | 0.27 | |||
| Vas | 3.7 | 13.70 | 0.00002 | ||||
| Post-Test | 0.45 | 20 | 0.49 | 0.11 |
Group B
| Mean | N | S.D | Std.Error
Mean |
Mean
Deference |
T | P | |
| Pre-test | 3.55 | 20 | 1.68 | 0.375 | |||
| vas | 3.15 | 7.5 | 0.00003 | ||||
| Post-test | 0.40 | 20 | 0.48 | 0.107 |
Between the group Group A
| Mean | N | S.D | Std.Error
Mean |
Mean
Deference |
T | P | |
| Pre-test | 4.15 | 20 | 1.24 | 0.27 | |||
| vas | 0.60 | 3.7 | 0.000062 | ||||
| Post-test | 3.55 | 20 | 1.68 | 0.375 |
Group B
| Mean | N | S.D | Std.Error
Mean |
Mean
Deference |
T | P | |
| Pre-test | 0.45 | 20 | 0.49 | 0.11 | |||
| vas | 0.05 | 0.322 | 0.0161 | ||||
| Post-test | 0.4 | 20 | 0.48 | 0.105 |
| Parameters | Group A | Group B |
| Pain(VAS) | 3.7 | 3.15 |
Interpretation
The above table shows the mean improvement in pain scores of VAS was 3.7 in group A and
3.15 in group B it was resulted that group A treated with core exercises with McKenzie method had a less effect in pain score over group B treated with core exercises with MFR in lumber disc prolapse in subjects.
RESULTS
This study concluded that core exercises with MFR had effective tool in lumbar disc prolapse stage 2 patients as reliving pain. While comparing with core exercises with McKenzie method.
DISCUSSION
Lumbar disc herniation is the most common diagnosis among the degenerative abnormalities of the lumber spine (effecting 2 to 3 percent of population) Greater risk of disc herniation has been attributed to smoking and exposure to repetitive loads and prolonged vibration. Conservative treatment is effective in 80% of patient with in 4 to 6 week.
Intervertebral discs can prolapse suddenly because of excessive pressure, examples include:
- Falling from a significant height and landing on your buttocks. This can transmit significant force across the spine. If the force is strong enough ether a vertebra can fracture, or an intervertebral disc can rupture.
- Banding forces places substantial stress on the vertebral discs. If you band and attempt to lift an object which is too heavy this force may cause a disc to rupture.
Intervertebral discs can also rupture as a result of weakening outer fibers of the disc. This is usually due to repetitive minor injuries build up over time. This damage may occur with aging, hereditary factors, work or recreation related activities.
A prolapsed disc can cause problem in two ways:
- Direct pressure – the disc material that has ruptured into the spinal canal or intervertebral foramen can put pressure on the nerves
- Chemical irritation – once ruptured, the core material of the disc can cause a chemical irritation of nerves roots and result in inflammation of the nerves.
In this study lumbar disc stage-2 patients were categories into 2 groups and one group treated with core exercises plus MFR method and other group treated with Mckenzie method plus MFR (myofascial release technique) various scale used to measure pain and statistical test used to interpret the data. This study shows that the core exercises plus MFR (myofascial release technique) has effective results on patients.
During myofascial release therapy the therapist locates myofascial areas that feel stiff and fixed instead of elastic and movable under light manual pressure these area, through not always near what feels like the source of pain are through to restrict muscle and joint movements, which contributes to wide spread muscle pain the focused manual pressure and stretching used in myofascial release therapy loosen up restricted movement, leading indirectly to reduced pain. In addition to core exercises it strengthen the back, as weak back leads to pain.
When core muscles are in poor condition, additional stress is applied to the spine as it supports the body, and back injury or back pain is more likely. Without specific back and abdominal exercises to target these muscles, they will naturally weaken over time, increasing the chance of developing or worsening back pain. Strong core muscles reduce the likelihood of back pain
episodes, reduce severity of back pain, improve posture, protect against injury by responding efficiently to stresses.
So core exercises with MFR techniques have effective results on patient. While other methods have no more effective on patients, because in MFR focused manual pressure loosen up restricted movements and core exercises strengthen the back muscles which reduce the pain. While other method not directly loose restricted movements and strengthen back.
Mckenzie method is a common intervention for patient with prolapse intervertebral disc.
Although this intervention sequence is effective but recurrence of symptoms is common, addition of core stabilization exercises will definitely give a permanent stability to disc thus reducing chances of recurrence.
Mckenzie with core strengthening exercises reduced pain improve strength, range of motion and reduces disability in P.I.V.D subjects.
The Mckezie method is successful with treating acute low back pain it is also very helpful for those patients with sub-acute and chronic back pain.
One of the benefits of the Mckenzie method is that it is a standardized approach to both the assessment and treatment of low back pain. The Mckenzie method is not simply a set of exercises; it is a defined algorithm that serves to classify the spinal problem so that it can be adequately treated. The Mckenzie method is grounded in findings a cause and effect relationship between the positions the patient usually assumes while sitting standing or moving and the generation of pain as a result of those positions or activities. The therapeutic approach requires a patient to move through a series of activities and test movements to gauge the patient’s pain response. The approach then uses that information to develop an exercise protocol designed to centralize or alleviate the pain.
Myofascial release (MFR) is a form of manual therapy that involves the application of a low load, long duration stretch to the myofascial complex, intended to restore optimal length, decrease pain and improve function.
Myofascial relese can help increase lymph and venous flow to promote the removal of exudates after an injury.
MFR therapy focuses on releasing muscular shortness and tightness many patient seek myofascial treatment after losing flexibility or function following an injury or if experiencing ongoing back, shoulder, hip or virtually pain in an area containing soft tissue.
CONCLUSION
The study on patients with stage-2 lumbar disc prolapse conclude that MFR (myofascial release technique) along with core exercises is more effective in alleviating primary symptoms of pain thus enhancing the functional capabilities of the patients.
LIMITATIONS AND RECOMMENDATION
Limitation
- duration of study is 3 months
- Study was undertaken for small sample size
Recommendation
- duration of study should be more
- Study should be taken for large sample size
REFERENCES
- Coulehan JL (1985) Adjustment, the hands and healing.Cult Med Psychiatry 9: 353- 382.
- Miller JK (1992) TheMcKenzie Approach. ClinOrthop 279: 8-20.
- Meszaros TF, Olson R, Kulig K, Creighton D, Czarnecki E (2000) Effect of 10%, 30%, and 60% body weight traction on the straight leg raise test of symptomatic patients with low back pain.J Orthop Sports PhysTher 30: 595-601.
- Wieting JM (2005) Massage, Traction, and Manipulation. Medscape.
- Werners R, Pynsent PB, Bulstrode CJ (1999) Randomised trial comparing interferential therapy with motorized lumbar traction and massage in management of low back pain in a primary care setting. Spine (Phila Pa 1976) 24: 1579-1581.
- Armstrong JR (1965) Lumbar disc lesions, (3rd edtn). Williams and Wilkins, Edinburgh, Livingstone.
- McKenzie RA (1981) The lumbar spine. Mechanical diagnosis and therapy. Spinal publications, Waikanae, NewZealand.
- Youssef J, Davidson B, Zhou BH, Lu Y, Patel V, et al. (2008) Neuromuscular neutral zones response to static lumbar flexion: Muscular stability compensator. ClinBiomech (Bristol, Avon) 23: 870-880.
- Laslett M (2009) Manual correction of an acute lumbar lateral shift: maintenance of correction and rehabilitation: a case report with video.J Man ManipTher 17: 78-85.
- McGill SM, Kippers V (1994) Transfer of loads between lumbar tissues during flexion- relaxation phenomenon. Spine (Phila Pa 1976) 19: 2190-2196.
- McKenzie RA (1972) Manual correction of sciatic scoliosis.N Z Med J 76: 194-199.
- Carroll LJ, Cassidy JD, cote P (2000) the Saskatchewan Health and Back Pain Survey: the prevalence and factors associated with depressive symptomatology in Saskatchewan adults. Can J Public Health 91: 459-464.Philadelphia Panel (2001)
- Philadelphia Panel Evidence-Based Clinical Practice Guidelines on Selected Rehabilitation Interventions for Low Back Pain. Phys Ther 81: 1641-1674.
- McKenzie RA, May S (2003) The Lumber Spine: Mechanical Diagnosis and Therapy (2nd edtn). Spinal Publications, Waikanae, New Zealand. Pellecchia GL (1994) Lumbar traction: a review of the literature.j Orthop Spotd Phys Ther 20: 262-267 Murrin KR, Rosen M (1985) Pain measurement, In: Smith G and Govindo BG (editors) Acute Pain: London: Butterworth.
- Kremer E, Atkinson JH, lgnelzi RJ (1981) measurement of Pain: Patient preference does not confound pain measurement.Pain 10:241-248.
- Revill Sl,Robinson JO, Rosen M, Hogg MI (1976) the reliability of a linear analogue for evaluating pain. Anaesthesia 31: 1191-1198.
- Vianin M (2008) Psychometric properties and clinical usefulness of the Oswestry Disability index. J Chiropr Med 7:161-163.
- Gordon SJ, Kish VL, et al. (1991) Mechanism of disc rupture. A preliminary report. Spine (Phila Pa 1976) 16: 450-456. Veres SP, Robertson PA, Broom ND (2008) ISSLS prize winner: Microstructure and mechanical disruption of the lumbar disc annulus:
- part II: how the annulus fails under hydrostatic pressure. Spine (Phila pa 1976) 33: 2711-2720.
- Donelson R, Aprill C, Medcalf R, Grant W (1997) A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine (Phila Pa 1976) 22: 1115-1122.
- Adams MA, May S, Freeman BJ, Morrison HP, Dolan P (2000) effects of backward bending on lumbar intervertebral disc. Relevance to physical therapy treatment for low back pain. Spine (phila pa 1976) 25: 431-437.
- Santolin SM (2003) McKenzie diagnosis and therapy in the evaluation and management of a lumbar disc derangement syndrome: A case study.J Chiropr Med 2: 60-65.
- Key JA, Ford LT (1948) Experimental intervertebral-disc lesions.J Bone Joint Surg Am 30A: 621-630.
- Melbye M (2010) An adherent nerve root–classification and exercise therapy in a patient diagnosed with lumbar disc prolapse.Man Ther 15: 126-129.
- Alfredson H, Pietilä T, Jonsson P, Lorentzon R (1998) Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis.Am J Sports Med 26: 360-366.
- Langberg H, Ellingsgaard H, Madsen T, Jansson J, Magnusson SP, et al. (2007) Eccentric rehabilitation exercise increases pe.
- John F.barnes,Pediatrics Myofascial release,Physical therapy forum- MRF techniques 1991
- Carol manhiann 2001.the myofascial release manual,3rd edition slack inc.
- Regi boehme,john boehme , myofascial release and its application to neuro development treatment 1991,page no.5-8,11-16,80.
- Keith Grant and Art Riggs. Modalities for massage and bodywork; Myofascial release; published by Massage Therapy Foundation 2005
- Wadell G. The back pain revolution, 2nd ed. Edinburg: Chruchill Livingstone, 2004:74
- Craig E. Morris, Low Back Syndromes,©2006,Epidemology of low back syndromes, pg 87
- Woolf A, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health
- Laura Punnett, Sc.D. et al. Estimating the global burden low back pain attributable to combined occupational exposures. American journal of industrial medicine,2005 dec;48(6):459-64
- AK Burton F;Balagué et al. European guidelines for management in low back pain; Eur Spine J. 2006 Mar;15Suppl 2:S136-68.
- Gordon Wadell. Nonorganic physical signs in low back pain;vol- 5(2),march/april 1980
- Andersson GBJ. The epidemiology of spinal disorders. The adult spine: principles and practice. 2nd ed. New York: Raven Press, 1997: 93- 141.
- Van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic non-specific low back pain: a systematic review of randomized controlled trials of the most common interventions. Spine 1997; 22:2128-2156.
- Travis Whitfill et al. Early Intervention Options for Acute Low Back Pain Patients:A Randomized Clinical Trial with One-Year Follow-Up Outcomes; J OccupRehabil (2010) 20:256–263
- Pengel LH, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: Systematic review of its prognosis. BMJ2003;327:323
- EdaGurcay et al. Acute LBP course and prognosis. Disability and Rehabilitation, 2009; 31(10): 840–845
- Christopher A Mayor; A meta analysis of massage therapy research. Psychological Bulletin Copyright 2004 by the American Psychological Association, Inc; 2004, Vol. 130, No. 1, 3–18.
- Manheim, C.J. The Myofascial Release Manual, third ed.Slack Incorporated, New Jersey, USA, 2001
- Robert Schleip. Fascial plasticity- a new neurobiological explanation: part 1; journal of bodywork and movement therapies(2003) 7(1), 11- 19.
- Paoloni J et al. Review of myofascial release as effective massage therapy technique; Athletic Therapy Today,2009,Sep;14(5):30-34
- The fascial network: an exploration of its load bearing capacity and its potential role as a pain generator, Robert Schleip, Fascia Research Project, Institute of Applied Physiology, Ulm University, Ulm, Germany
- Norkin C.C, Levangie PK, Joint structure and function, 4thed, Jaypee brothers medical publication, 2006
- I A Kapanji. The physiology of joints;2nd edition vol-3; Edinburg London &New York 1974
- John Barnes, PT. Myofascial release approach: part 1; massage magazine, dec 2006.
- Pathophysiology of pain and pain assessment. American medical association©2010
- Craig E. Morris, Low Back Syndromes, ,Myofascial release in low back syndromes,©2006 pg 243-276
- Panjabi MM 2006 A hypothesis of chronic low back pain: ligament subfailure injuries lea to muscle control dysfunction; Eur spine J 15(5): 668-76
- Schleip R, et al. 2007 Letter to the Editor concerning “A hypothesis of chronic backpain: ligament subfailure injuries lead to muscle control dysfunction” (M.Panjabi). Eur Spine J 16: 1733-35
- Paolo Tozzi.Fascial release effects on patients with non-specific cervical or lumbar pain; Journal of Bodywork & Movement Therapies (2011) 15, 405e416
- Taguchi, T., et al. The thoracolumbar fascia as a source of low back pain. In P.A. Huijing et al. (Eds.), Fascia ResearchII: Basic Science and Implications for Conventional and Complementary Health Care. Munich, Germany: Elsevier 2009
- Lieutenant Colonel Joseph R. et al. The effects of spinal flexion and extension exercises and their associated postures in patients with acute low back pain;Spine J vol20, no.21. pg 2303-2312.
- Michael Vianin DC. Psychometric properties and clinical usefulness of the Oswestry Disability Index;; Journal of Chiropractic Medicine (2008) 7, 161–163 Pedretti L W, Occupational therapy practice skills for physical dysfunction, 4thed, 1996, pg 87-88.
- Danniel&Worthighams, Techniques of manual examination, 6th edition
- Marshall P. W., Murphy BA. Evaluation and neuromuscular changes after exercises rehabilitation for low back using a swiss ball: a pilot study. Journal of Manipulative physiotherapy, 2006 sept, 29 (7) 550- 560
- D. J. L. Kuh. Height, occupation and back pain in a national prospective study; British Journal of Rheumatology 1993;32:911-916
- Michael Pfingsten. Fear avoidance behavior and anticipation of pain in patients with chronic low back pain;
- Jonathan R Field1*, Field et al. Preliminary study into the components of the fear- avoidance model of LBP: change after aninitial chiropractic visit and influence on outcome. Chiropractic & Osteopathy 2010, 18:21
- Swinkels-Meewisse IE. Fear-avoidance beliefs, disability, and participation in workers and non-workers with acute low back pain;Clin J Pain. 2006 Jan;22(1):45-54
- Hernandez-Reif M. Lower back pain is reduced and range of motion increased after massage therapy; Int J Neurosci. 2001;106(3-4):131- 45.
- Rose Adams. The Effects of Massage Therapy on Pain Management in the Acute Care Setting; Int J Ther Massage Bodywork. 2010; 3(1): 4– 11.
- Paul Dolder et al. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain;; Australian journal of physiotherapy 49: 183-188.
- www.pubmed.com
- www.google.com
LIST OF ABBREVIATION
V.A.S – VISUAL ANALOGUE SCALE
M.M.T – MANUAL MUSCLE TESTING
O.Q.D – OSWESTRY DISABILITY QUESTIONNAIRE
M.F.R – MYOFASCIAL RELEASE
Comparison between the effects of core exercises with Mckenzie method versus core exercises with Myofascial release Technique in stage – 2 of lumbar disc prolapse
Dr. Manash Kanti Chakraborty, MPT Ortho, Deepika Tanwar, MPT Ortho
ABSTRACT
STUDY OBJECTIVES: Comparison between the effects of core exercises with Mckenzie method versus core exercises with Myofascial release Technique in stage – 2 of lumbar disc prolapse.
DESIGN: Pre-test and post-test two group comperative study design. PARTICIPANTS: Thirty subjects aged 30-50 years with clinically diagnosed as stage -2 lumbar disc prolapse were selected under randomized sampling technique and assigned in to two groups with 15 subjects each, one group received core exercises with Mckenzie method and other group core exercises with Myofascial release Technique for a period of 12 weeks.
OUTCOME MEASURES: Visual Analogue Scale (VAS) and Oswestry Disability Questionnaire (ODQ)
RESULT: Patients in core exercises with Myofascial release group shows significantly better than core exercises with Mckenzie method group.
KEY POINT: Core Exercises, Mckenzie method, Myofascial release technique, stage – 2 of lumbar disc prolapse.
INTRODUCTION
A prolapsed lumbar disc is a spine condition that can cause lower back pain, numbness, tingling and muscle weakness in the lower body.it can happen to people of all ages, but becomes more common after the age of 35.
Herniated lumbar disc material (nucleus pulposus or annulus fibrosus) beyond the intervertebral disc space. The highest prevalence is among people aged 30-50 years, with a male to female ratio of 2:1. In people aged 25-55 year, about 95% of herniated discs occur at the lower lumbar spine (l4/5andl5/s1 levels); disc herniation abovet his level is more common in people aged over 55 years.
A prolapsed lumbar disc can occur anywhere in the lumbar region of the spine, specially the vertebrae at the base the disc between these relatively flexible lumbar vertebrae prone to prolapse because the lower back support much of the body’s weight.
As the body ages the discs between our vertebrae begin to lose their elasticity and their ability to bounce back from everyday movement .this creates pressure which pushes the soft inner disc against the fibrous outer layer. Eventually the disc wall can tear and inner material pushes into the spinal column, resulting in a prolapsed disc.
International surveys of low back pain reported that one month prevalence was 19 – 43 % and point prevalence was 15 – 30 %.
The estimated worldwide life time prevalence of low back pain varies from 50 – 84 % .
Experts estimate up to 80% of population will experience back pain at some time of their lives. Worldwide, years lived with disability caused by low back pain have increased by 54
% between 1990 and 2015.
In India over all the prevalence of low back pain found to be 42%. The majority of women (60.9%) with low back pain experienced moderate disability . prevalence of low back pain among women was comparatively more then other studies in India.
There are many back pain myths
- Myth: always sit up straight
Fact: slouching is bad, but sitting up too straight and still for long periods can also be a strain on back.
- Myth : don’t lift heavy things.
Fact : it’s not necessarily how much you lift it’s how you do it .
- Myths : bed rest is the best cure.
Fact : yes, resting can help a recent injury or strain that causes back pain, but a day or two in bed can actually make it worse.
- Myth : exercise is bad for back pain.
Fact : regular exercise prevent back pain.
- Myth : firmer mattresses are better. Fact : medium firm mattress hurt less.
TheMcKenziemethodisaclassificationsystemandaclassificationbasedtreatmentfor patients withlowbackpain. Aacronymfor the Mc Kenziemethodismechanical diagnosis and therapy (MDT) the M c Kenzie method was developed in 1981 byrobin Mc. Kenzie a physical therapist from new Zealand .
Mckenzie exercise are designed to reposition any displaced intervertebral disc. This is initially done by using gravity to draw the disc back into the spine and then actively consolidate the effect of gravity. To facilitate disc movement, when performing the exercise and maintain relaxed and even breathing for the duration of exercise.
The Mckenzie method also referred to as mechanical diagram and therapy is a method of assessing and treating spinal back join and related extremity pain most commonly through the use of specific repeated movements and appropriate prevention measures. The method puts an emphasis on self-core after initial clinical visits it uses primarily self-treatment strategies and minimizes manual therapy procedure with the Mc.kenzie trained therapist supporting the patient with passive procedures only if an individual self- treatment program is not fully effective.
The Mckenzie method also referred to as mechanical diagnosis and therapy is a method of assessing and treating spinal back pain and related extremity pain most commonly through the use of specific repeated movements and appropriate prevention measures.
Centralization – centralization occurs when pain symptoms off-centered from the mid-line of the spine often diagnosed as sciatica, migrate towards the centre of mid-line of the spine this migration of pain symptoms to the centre of lower back is a sign of progress in the Mckenzie method. The most common directional preference that result in centralization is extension of the back.
Classification – there are three primary classification that results from the assessment portion of the Mckenzie method comprehensive approach ; postural syndrome, dysfunction syndrome and derangement syndrome.
Derangement syndrome – the most common treatment classification defined by pain that is experienced due to a disturbance in the joint area resulting in diminished movement in certain directions.
Dysfunction syndrome – this type of pain is categorized by mechanical impairments and deformities of impaired tissue within the body.
Postural syndrome – this type of pain is the result of postural deformation position such as slouching are the cause of postural syndrome.
The McKenzie method exists of 3 steps
- Evaluation
- Treatment
- Prevention
The evaluation is received using repeated movements and sustained positions, with the aim to elicit a pattern of pain responses called centralization .The symptoms of lower limb and lower back are classified into three sub groups: derangement syndrome, dysfunction syndrome and postural syndrome.
The prevention step consist of encouraging the patient to exercise regularly and self-care. The choice of exercises in the McKenzie method is based upon the direction (flexion,
extension or lateral shift of the spine)
The McKenzie method educates patients regarding movement and position strategies can reduce pain.
Principle –
- Kyphotic antalgic management: extension principle
- Acutec or on a lantalgic management: lateral flexion– then– extension principle
- Acute lordotic antalgic management: flexion principle.
Core exercises are a crucial part of any exercise regimen. These exercises strengthen the body, particularly the pelvis hip and lower back areas.
Some examples of this type of exercise include crunches, reverse crunches, ball crunches, and oblique
Crossing over crunches air bicycling plank, butt lifts, back extension with ball and many more.
These exercises work on the deep abdominal muscles, strengthen abs and flatten them, core exercises also make the lower back stronger and healthier.
Doing core exercises stimulates a particular area in the brain called the cerebellum that links to body parts for coordination, spatial awareness.
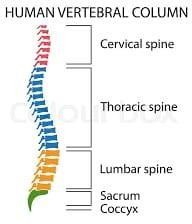
Figure No.1

Figure No.2
Mckenzie exercises may be effective in decreasing symptoms, specially leg pain.
Mckenzie exercises centralize back pain, moving it from the leg to the lower back with daily exercises that works to relive acute or chronic pain.
Core exercises support lower back in herniated disc. Core exercises work on lower abdominal muscles.
Core exercises cause flexibility of Spine, give power to muscles provide balance and stability of lower back decrease lower pain and injury.
Core stability is the term used to describe the muscular control required to maintain functional stability around the lumber spine and to prevent lower back pain.
The “core” is often mistaken for the visible abdominal muscles the rectus abdomens, the “abs”, however, the muscles involved can be described as a muscular box and include abdominals in the front (rectus abdominus , transverse abdominus , multifedus, internal oblique) paraspinals and gluteals in the back the diaphragm at the top and the peluic floor on the bottom.
Myofascial release Technique(MFR):
Myofascial release is an alternative medicine therapy that claims to treat skeletal muscle immobility and pain by relaxing contracted muscles, improving blood and lymphatic circulation , and stimulating the stretch reflex in muscles.
The approach was promulgated as an alternative medicine concept by Andrew Toylor still, inventor of osteopathy. The exact phrase “ myofascial release” was coined in the 1960s by Robert ward, an osteopath who studied with Ida Rolf, the originator of rolfing word , along with physical therapist Johan Barnes, are considered the two primary founders of Myofascial release.
Step I: Getting Ready
Step II: Thelengthening processes Step III: Completion
Step IV: Postural integration
Myofascial release is a system of diagnosis and treatment first described by Andrew Taylor still and his early students, which engages continual palpatory feedback to achieve release of myofacial tissues.
Myofascial release techniques have been anecdotally reported as being effective in reliving restrictions and increasing range of motion. Direct MFR techniques engage the restrictive barrier and the tissue is then loaded with a constant force until tissue release/relaxation occurs.
Indirect MRF involves gliding the dysfunctional tissues along the path of least resistance
(away from the barrier) until free movement is achieved.
The goals of myofascial treatment include relaxation of contracted muscles increased circulation to an area of ischemia increase venous and lymphatic drainage and the stimulation of stretch reflexes in hypotonic muscle.
NEED OF THE STUDY
The results of the study may help the physiotherapists to identify and use the appropriate methods in the treatment of stage-2 lumbar disc prolapse patients. This study can also help the physiotherapists in understanding the relation between the different parameters considered for the study under such as VAS (Visual analogue Scale), MMT (Manual muscle Testing), spinal ranges. The study provides an information, that how the study will contribute and who will benefit for it. It includes an explanation of the study’s importance as well as its benefits. By evaluating the results of the study, the physiotherapist able to identify the positive outcomes. The study can help the physiotherapist what impact will these treatment have upon reducing the patient’s problem and promoting health.
With the Mckenzie approach, physical therapy and exercise used to extend the spine can help “centralize” the patient and pain by moving it away from the extremities (leg or arm) to the back.
The long term goal of Mckenzie method is to teach patients suffering from back pain how to treat themselves and manage pain throughout their lives using exercise and other strategies.
Whereas strong core may actually help prevent back pain by making less prone to back injuries and proper spinal alignment. Strengthening core muscles may also help improve back pain.
The focused manual pressure and stretching used in myofascial release therapy loosen up restricted movement leading to reduced pain.
The core exercises with Mckenzie method and core exercises with MFR technique are used in this study to treat the patients and compare the effects of both techniques, because of its effectiveness, easy to understand by the patients, less time consuming and cost effective. Seong Hun Yu, Yong Hyeon Sim, and Hyun Jin kim study the effects of abdominal drawing in exercise and myofascial release on pain flexibility and balance of elderly females who complained of low back pain.
The abdominal drawing in exercise group show significant difference in pain & balance and myofascial release group show significant deference in pain & flexibility after exercise. Macey Berube, BS, in his case report found Mckenzie exercise with core strengthening shows improvement in pain & activity levels motion strength and tenderness.
AIMS OF THE STUDY
To evaluate the comparison of core exercises with McKenzie method in stage-2 lumbar disc prolapse patients. To find the effects of core exercises with Myofascial release Technique in stage- 2 lumbar disc prolapse patients. To compare between the effects of core exercises with Mckenzie method versus core exercises with Myofascial release Technique in stage – 2 of lumbar disc prolapse.
OBJECTIVE OF STUDY
- To evaluate the effects of different exercises
- To compare between the effects of different exercises
- To find out new facts if any at any stage
- To find out the limitations and recommendations
- To verify and test important facts
- To find solution to problem
HYPOTHESIS
Alternate hypothesis:
There is significant difference between the effect of core exercises with McKenzie method and the effect of core exercises with MFR in stage-2 lumbar disc prolapse patients
Null hypothesis:
There is no significant difference between the effect of core exercises and core exercises with Mckenzie method in patient with stage- 2 lumbar disc prolapse.
MATERIALS
Materials used:
- Couch : used for treatment and comfortable position of the patients
- Timer : used to note the treatment time
- Pillows : used to support body parts
- Goniometer: used to measure range of motion of joints
- Paper
- Pencils
- Duly signed Consent forms
OUTCOME MEASURE
- VISUAL ANALOGUE SCALE (VAS)
OSWESTRY DISABILITY QUESTIONNAIRE (ODQ)
METHODOLOGY
STUDY DESIGN
This study design involving the comparative analysis of two groups treated with core exercises with McKenzie method and core exercises with Myofascial release Technique respectively and assessed by VAS (Visual analogue Scale), MMT (Manual muscle Testing) ,spinal ranges.
SAMPLE SIZE:
Fourty subject with stage-2 lumbar disc prolapse aged between 30-50 years were selected according to convenience (purposive) sampling based on the selection criteria.
These subject were then randomly assigned into two groups of twenty subjects each namely experimental group A and experimental group B.
All the participants took part in the experiment on a voluntary basis after signing a consent from and a demographic data was collected from each subject. The purpose of the study was explained to all the subjects.
SAMPLING METHOD: Experimental method STUDY CENTRE: College Opd Dabok INCLUSION CRITERIA:
- Patients clinically diagnosed as stage -2 lumbar disc prolapse.
- Age group from 30-50 years.
EXCLUSION CRITERIA:
- Patients with grade 3, 4 lumbar disc prolapse.
- Age less than 30 and more than 50 years. History of any recent spine surgery.
- History of any spinal diseases.
STUDY DURATION:
- Total duration of study: 12 weeks
- Sessions:1 Session per day
- Duration of sesson:15 to 30 minutes
- Days per week:5 days a week
MEASUREMENT TOOLS:
- Visual analogue scale(VAS)
- Manual muscle testing (MMT)
- Spinal ranges
- Oswestry disability questionnaire(ODQ)
Visual analogue scale(VAS): It was used for pain assessment where by pain was rated from 0
– 10 in which the ‘0’ represented no pain and 10 represented maximum pain tolerance subject were indicated the best number for their pain.
Manual muscle testing (MMT): Manual muscle tests are performed daily by Physiotherapists not only is it used to help predict a patients ability to function it provides a reference with which to document progress.
Grades of MMT-
- none – no visible or palpable contraction
- trace – visible or palpable contraction with no motion. 2 poor – full ROM gravity eliminated
3 fair – full ROM against gravity
good – full ROM against gravity, moderate resistance. 5 normal – full ROM against gravity, maximal resistance .
Spinal ranges – the lumbar spine commonly known as the low back is also tested during range of motion exams the lumbar spine has five vertebrae and connects the spine to the pelvis normal lumbar ranges of motion include 60 degree of flexion 25 degree of extension and 25 degree of lateral or side bending .
Oswestry disability questionnaire (ODQ) : ODQ was completed to assesses percentages of functional disability in patients with lumbar disc prolapse this questionnaire is a gold standard tool indicate ability of patients with lumbar disc prolapse . it consist of 10 section and each of the section includes 6 rates from 0-5. The first section of this questionnaire rates pain and the other section assesses activities of daily living total score of questionnaire was recorded as percentage.
PROCEDURE
40 subject clinically diagnosed as stage-2 lumbar disc prolapse was selected according to inclusion and exclusion criteria and divided randomly into two groups ; namely experimental group A and experimental group B, consisting of 20 subject each.
A brief explanation about the treatment session will explained to all the subjects. The treatment duration for both the group will given as listed below:
Duration per session: 15-30 minutes /session No. of session per day : 1session /day No. of days per week : 5 days a week Duration of the study : 3 months
The visual analogue scale, manual muscle testing , spinal ranges and oswestry disability questionnaire were noted before and at the end of 4th week of treatment group A will treated with core exercises and Mckenzie method group B received core exercises with myofascial technique.
Group A (core exercises with Mckenzie methods): the subject will in a comfortable position support your lower back by sitting upright in a firm chair place feet firmly on floor. Tighten abdominal muscles and bring belly button toward the back of the chair. Hold this tension for 10 seconds.
Bird dog – start on all four limbs and extend the left leg behind you while extending the right arm in front with your thumb up. Compress your abdominal muscles and hold for 10-20 seconds then repeat on the opposite side.
Plank – plank is basically the position in when you are at the top of a push-up. Hold it as long as possible, drawing in your stomach and compressing your lower abs.
Abdominal draw – in supine position drawing the lower abdomen in and then drawing up the pelvic floor muscle so that it contract together with their lower abdomen.
McKenzie exercises fall into 2 categories with opposite movement extension and flexion. Extension and flexion exercises involve moving the spine in opposite directions. Extension exercises by moving spine backward, which is spinal extension. Lie on your abdomen and work up to raising your head and chest off the floor to prop yourself up onto your elbow flexion exercises involve bending the spine forward, in the opposite direction as spinal extension . flexion exercises can be perform by seated standing or lying on back . bringing knees to your chest while lying down is an example of a lying flexion exercise. (Reference No.14)
Group B core exercises with MFR (Myofascial release technique): core exercises are mention above with MFR (Myofascial release technique)
- Land on the surface of the body with the appropriate “tool” (knuckles, or forearm tc)
- Sink in to the soft tissue.
- Contact the first barrier/restricted layer.
- Put in a “line of tension”.
- Engage the fascia by taking up the slack in the tissues.
- Finally move or drag the fascia across the surface while staying it touch with the underlying layers.
- Exit gracefully.
- Data collection-
All the data was collected with outcome measure and kept safely for statistical analysis.
- Statistical test-
An appropriate statistical tests will be applied to the data for analysis.
- Limitation-
Will be able to present only after the detail study has been carried out.

Figure No.3 McKenzie extension exercise

Figure No.4 McKenzie extension exercise

Figure No.5 Bridging exercise

Figure No.6 Plank variation

Figure No.7 Myofascial release technique

Figure No.8 Myofascial release technique

Figure No.9 Myofascial release technique

Figure No.10 Myofascial release technique
DATA ANALYSIS
Pre-test and post test data within group and between group well be analyses by paired and un paired ‘t’ test.
The differences between pre test and post test values were found the mean deference VAS of A compared with group B and the actual pattern of variation were observed.
With the ‘t’ value from the pre test and post test the accurate level of significance was analyses and interpreted.
An alpha level of p < 0.05 was the level of significant for the test Arithmetic mean: –
X̅ =∑x∕N Where,
X = Arithmetic mean
∑x= sum of all variables
N= total number of variables Standard deviation (s.d)
s.d= √(X-X̅ )2 /√N where,
x̅ = mean of scores
X = sum of all variable N = total no of variables (X-X̅ ) = deviation
Paired ‘t’ Test within group:
The paired ‘t’ test was used to find out the significance within the same group with the values of parameters considered for the study.
The formula to find the value of “t” using paired ‘t’ test:
t= [M1-M2]/SEMd
Where,
M1= Mean 1
M2= Mean 2
SEMd= Standard error of mean difference SEMd= √SEM12 + SEM22 – 2r SEM1 SEM2
r=correlation between GROUP A and GROUP B df=N-1
UNPAIRED ‘t’ TEST BETWEEN GROUP:
The ‘t’ test was used to find out the significance between the groups and it gives the variable information regarding this study.
The formula to find the value of ‘t’ using unpaired ‘t’ test for GROUP A via GROUP B: t=[M1-M2]/SEMd
where,
M1= Mean 1 M2 = mean 2
SEMd=Standard error of mean difference SEMd =√SEM12 +SEM22
SEM1 = Ꝺ1/√N1 SEM2= Ꝺ2/√N2
Demographic presentation of data in group
40 subject of age group 30-50 years were randomly selected according to inclusion and exclusion criteria and divided into two group with 20 subjects in each group. group A had a mean age of 38.6 years and group B had a mean age of 41.9 the demographic data of both the groups has been presented in table 5.1.
Table 5.1 demographic presentation of data in graph:
| Age in year | ||||
| Group | Number | Mean | S.D | |
| Group A | 20 | 38.6 | 6.40 | |
| Group B | 20 | 41.9 | 6.17 | |
| Total | 40 | 40.25 | 6.506 | |
Demographic presentation of data in group
Graph
45
41.9
40
38.6
35
30
25
20
15
10
6.4
6.17
5
0
Group A
Group B
Group A Group B
Figure:5.1
Analysis of pre-test and port-test value of pain using visual analogue scale (VAS) for significance within Group A:
The pain score due to lumber disc prolapse of each subject in group A was assessed by using visual analogue scale (V.A.S) before the start of the treatment as pre-test values and at the end of 3rd month as post-test values the data has been presented in table and depicted in figure 5.2
Table:5.2 analysis of pre-test and post-test values of pain scores using visual analogue scale (VAS)
For significance within group A.
| Mean | N | S.D | Std Error
Mean |
Mean Deference | T | P | Significance | |
| Pre-test | 4.15 | 20 | 1.24 | 0.27 | ||||
| VAS | 3.7 | 13.70 | 0.00002 | significant | ||||
| Post-test | 0.45 | 20 | 0.49 | 0.11 |
Interpretation – the above table shows the mean of pre-test and post-test VAS values were 4.15 and 0.45 respectively. the mean improvement in pain scale of groups was 3.7 the ‘t’ value 13.70 and ‘p’ values 0.00002 for pain scores using VAS within group A analysis.
When compared to table value . the above ‘P’ value is lesser at p < 0.05 which is significant it indicate that group A treated with core exercises with Mckenzie method had less significant in pain intensity.
Analysis of pre-test and post test values of pain scores using visual analogue scale (VAS) for significance with group B:
The pain sore due to lumber disc prolapse of each subject in group B was assessed by using visual analogue scale (VAS) before the start of the treatment as pre-test values and at the end of 3rd month as post test value the data has been presented in table 5.3 and depicted in figure 5.3
Table 5.3 analysis of pre-test and post test values of pain scores using visual analogue scale (VAS) for significant within group B.
| Mean | N | S.D | Std.Error
Of Mean |
Mean
Difference |
T | P | Significance | |
| Pre-test | 3.55 | 20 | 1.68 | 0.375 | ||||
| VAS | 3.15 | 7.5 | 0.00003 | significant | ||||
| Post-test | 0.4 | 10 | 0.48 | 0.107 |
Interpretation – the above table shows the mean of pre-test and post-test VAS values were 3.55 and 0.4 respectively the mean improvement in pain score group b was 3.15 the ‘t’ value 7.5 and ‘P’ value 0.00003 for pain score using VAS within group B analysis when compared to table value , the above ‘p’ value is lesser at p<0.05 which is significant. It indicates that group B treated with core exercise with MFR had significant improvement effect in pain intensity .
Fig 5.2 . analysis of pre-test and post-test values of pain scores using visual analogue scale (VAS) for significant within group A.
Chart Title
4.5
4.15
4
3.5
3
2.5
2
1.5
1.24
1
0.45 0.49
0.5
0
pre-test
post-test
Series 1 Series 2
Figure 5.3 analysis of pre-test and post-test values of pain scores using visual analogue scale (VAS) for significant within Group B
Chart Title
4
3.55
3.5
3
2.5
2
1.5
1
0.5
0
Pre-test
Post-test
Series 1 Series 2
| 1.68 | 0.4 0.48 | |||||
Analysis of Pre-test values of pain scores using VAS of lumber disc proper between group
The pain score of lumber disc prolapse of each subject in group A and group B were assessed by using visual analogue scale (VAS) before the start of the treatment as pre-test values .the values of group A & group B were compared between groups for significance of treatment the data has been presented in table 5.4.
Tables 5.4 Analysis of pre-test values of pain scores using VAS for significance between group.
| Group | Mean | N | S.D | Std Error
Of Mean |
Mean
Deference |
T | P | Significance | |
| VAS | A | 4.15 | 20 | 1.24 | 0.27 | ||||
| 0.60 | 3.7 | 0.000062 | significant | ||||||
| Pre-test | B | 3.55 | 20 | 1.68 | 0.375 |
Interpretation
The above table shows the mean of free test values of pain scores were 4.15 and 3.55 in group A and group B respectively .the mean deference in pain scores between group were 0.60 . the ‘t’ value 3.7 and ‘P’ value 0.00062 for pain scores of lumbar disc prolapse between group a and group B analysis when compared the table value the above ‘P’ value is lesser at p < 0.05 which is significant ,
Analysis of post-test values of pain scores using VAS of lumbar disc prolapse between groups.
The pain scores of lumbar disc prolapse of each subject in group a and group b were assist by using VAS at the end of third month as post-test values. The value of group a and group b were compared between group for significance of treatments .
Analysis of post test values of pain scores using VAS for significance between groups
| Group | Mean | N | S.D | Std.Error Mean | Mean Deff. | T | P | Significance | |
| VAS
Post- Test |
A | 0.45 | 20 | 0.49 | 0.11 | ||||
| 0.05 | 0.32
2 |
0.016 | Non-
Significant |
||||||
| B | 0.4 | 20 | 0.48 | 0.105 |
Interpretation the above table show the post-test value for group a and group b of mean 0.45 and 0.4 respectively and ‘t’ value 0.322 for pain score using VAS between groups. When compared to table value, the above p value is 0.016 at p < 0.05, which is greater it indicates that technique were effective in lumber disc prolapse but the group A treated with core exercises with Mckenzie method has less effect then group B treated with core exercise MFR in subjects
Mean improvement in all the parameter between group A and group B
The pain score of each subject in group A and group B were assessed by using VAS before the start of the treatment and at the end of third month the mean improvement in pain score were compared between both the group.
| Group | Mean | N | S.D | Std Error
Of Mean |
Mean
Deference |
T | P | Significance | |
| VAS | A | 4.15 | 20 | 1.24 | 0.27 | ||||
| 0.60 | 3.7 | 0.000062 | significant | ||||||
| Pre-test | B | 3.55 | 20 | 1.68 | 0.375 |
Interpretation
The above table shows the mean of free test values of pain scores were 4.15 and 3.55 in group A and group B respectively .the mean deference in pain scores between group were 0.60 . the ‘t’ value 3.7 and ‘P’ value 0.00062 for pain scores of lumbar disc prolapse between group a and group B analysis when compared the table value the above ‘P’ value is lesser at p < 0.05 which is significant ,
Analysis of post-test values of pain scores using VAS of lumbar disc prolapse between groups.
The pain scores of lumbar disc prolapse of each subject in group a and group b were assist by using VAS at the end of third month as post-test values. The value of group a and group b were compared between group for significance of treatments .
Analysis of post test values of pain scores using VAS for significance between groups
| Group | Mean | N | S.D | Std.Error Mean | Mean Deff. | T | P | Significance | |
| VAS
Post- Test |
A | 0.45 | 20 | 0.49 | 0.11 | ||||
| 0.05 | 0.32
2 |
0.016 | Non-
Significant |
||||||
| B | 0.4 | 20 | 0.48 | 0.105 |
Interpretation the above table show the post-test value for group a and group b of mean 0.45 and 0.4 respectively and ‘t’ value 0.322 for pain score using VAS between groups. When compared to table value, the above p value is 0.016 at p < 0.05, which is greater it indicates that technique were effective in lumber disc prolapse but the group A treated with core exercises with Mckenzie method has less effect then group B treated with core exercise MFR in subjects
Mean improvement in all the parameter between group A and group B
The pain score of each subject in group A and group B were assessed by using VAS before the start of the treatment and at the end of third month the mean improvement in pain score were compared between both the group.
| Group | No | Age In Years | |
| Mean | S.D | ||
| Group A | 20 | 38.6 | 6.40 |
| Group B | 20 | 41.9 | 6.17 |
| Total | 40 | 40.25 | 6.506 |
Within group:
Group A
| Mean | N | S.D | Std.Error
Mean |
Mean
Difference |
T | P | |
| Pre-Test | 4.15 | 20 | 1.24 | 0.27 | |||
| Vas | 3.7 | 13.70 | 0.00002 | ||||
| Post-Test | 0.45 | 20 | 0.49 | 0.11 |
Group B
| Mean | N | S.D | Std.Error
Mean |
Mean
Deference |
T | P | |
| Pre-test | 3.55 | 20 | 1.68 | 0.375 | |||
| vas | 3.15 | 7.5 | 0.00003 | ||||
| Post-test | 0.40 | 20 | 0.48 | 0.107 |
Between the group Group A
| Mean | N | S.D | Std.Error
Mean |
Mean
Deference |
T | P | |
| Pre-test | 4.15 | 20 | 1.24 | 0.27 | |||
| vas | 0.60 | 3.7 | 0.000062 | ||||
| Post-test | 3.55 | 20 | 1.68 | 0.375 |
Group B
| Mean | N | S.D | Std.Error
Mean |
Mean
Deference |
T | P | |
| Pre-test | 0.45 | 20 | 0.49 | 0.11 | |||
| vas | 0.05 | 0.322 | 0.0161 | ||||
| Post-test | 0.4 | 20 | 0.48 | 0.105 |
| Parameters | Group A | Group B |
| Pain(VAS) | 3.7 | 3.15 |
Interpretation
The above table shows the mean improvement in pain scores of VAS was 3.7 in group A and
3.15 in group B it was resulted that group A treated with core exercises with McKenzie method had a less effect in pain score over group B treated with core exercises with MFR in lumber disc prolapse in subjects.
RESULTS
This study concluded that core exercises with MFR had effective tool in lumbar disc prolapse stage 2 patients as reliving pain. While comparing with core exercises with McKenzie method.
DISCUSSION
Lumbar disc herniation is the most common diagnosis among the degenerative abnormalities of the lumber spine (effecting 2 to 3 percent of population) Greater risk of disc herniation has been attributed to smoking and exposure to repetitive loads and prolonged vibration. Conservative treatment is effective in 80% of patient with in 4 to 6 week.
Intervertebral discs can prolapse suddenly because of excessive pressure, examples include:
- Falling from a significant height and landing on your buttocks. This can transmit significant force across the spine. If the force is strong enough ether a vertebra can fracture, or an intervertebral disc can rupture.
- Banding forces places substantial stress on the vertebral discs. If you band and attempt to lift an object which is too heavy this force may cause a disc to rupture.
Intervertebral discs can also rupture as a result of weakening outer fibers of the disc. This is usually due to repetitive minor injuries build up over time. This damage may occur with aging, hereditary factors, work or recreation related activities.
A prolapsed disc can cause problem in two ways:
- Direct pressure – the disc material that has ruptured into the spinal canal or intervertebral foramen can put pressure on the nerves
- Chemical irritation – once ruptured, the core material of the disc can cause a chemical irritation of nerves roots and result in inflammation of the nerves.
In this study lumbar disc stage-2 patients were categories into 2 groups and one group treated with core exercises plus MFR method and other group treated with Mckenzie method plus MFR (myofascial release technique) various scale used to measure pain and statistical test used to interpret the data. This study shows that the core exercises plus MFR (myofascial release technique) has effective results on patients.
During myofascial release therapy the therapist locates myofascial areas that feel stiff and fixed instead of elastic and movable under light manual pressure these area, through not always near what feels like the source of pain are through to restrict muscle and joint movements, which contributes to wide spread muscle pain the focused manual pressure and stretching used in myofascial release therapy loosen up restricted movement, leading indirectly to reduced pain. In addition to core exercises it strengthen the back, as weak back leads to pain.
When core muscles are in poor condition, additional stress is applied to the spine as it supports the body, and back injury or back pain is more likely. Without specific back and abdominal exercises to target these muscles, they will naturally weaken over time, increasing the chance of developing or worsening back pain. Strong core muscles reduce the likelihood of back pain
episodes, reduce severity of back pain, improve posture, protect against injury by responding efficiently to stresses.
So core exercises with MFR techniques have effective results on patient. While other methods have no more effective on patients, because in MFR focused manual pressure loosen up restricted movements and core exercises strengthen the back muscles which reduce the pain. While other method not directly loose restricted movements and strengthen back.
Mckenzie method is a common intervention for patient with prolapse intervertebral disc.
Although this intervention sequence is effective but recurrence of symptoms is common, addition of core stabilization exercises will definitely give a permanent stability to disc thus reducing chances of recurrence.
Mckenzie with core strengthening exercises reduced pain improve strength, range of motion and reduces disability in P.I.V.D subjects.
The Mckezie method is successful with treating acute low back pain it is also very helpful for those patients with sub-acute and chronic back pain.
One of the benefits of the Mckenzie method is that it is a standardized approach to both the assessment and treatment of low back pain. The Mckenzie method is not simply a set of exercises; it is a defined algorithm that serves to classify the spinal problem so that it can be adequately treated. The Mckenzie method is grounded in findings a cause and effect relationship between the positions the patient usually assumes while sitting standing or moving and the generation of pain as a result of those positions or activities. The therapeutic approach requires a patient to move through a series of activities and test movements to gauge the patient’s pain response. The approach then uses that information to develop an exercise protocol designed to centralize or alleviate the pain.
Myofascial release (MFR) is a form of manual therapy that involves the application of a low load, long duration stretch to the myofascial complex, intended to restore optimal length, decrease pain and improve function.
Myofascial relese can help increase lymph and venous flow to promote the removal of exudates after an injury.
MFR therapy focuses on releasing muscular shortness and tightness many patient seek myofascial treatment after losing flexibility or function following an injury or if experiencing ongoing back, shoulder, hip or virtually pain in an area containing soft tissue.
CONCLUSION
The study on patients with stage-2 lumbar disc prolapse conclude that MFR (myofascial release technique) along with core exercises is more effective in alleviating primary symptoms of pain thus enhancing the functional capabilities of the patients.
LIMITATIONS AND RECOMMENDATION
Limitation
- duration of study is 3 months
- Study was undertaken for small sample size
Recommendation
- duration of study should be more
- Study should be taken for large sample size
REFERENCES
- Coulehan JL (1985) Adjustment, the hands and healing.Cult Med Psychiatry 9: 353- 382.
- Miller JK (1992) TheMcKenzie Approach. ClinOrthop 279: 8-20.
- Meszaros TF, Olson R, Kulig K, Creighton D, Czarnecki E (2000) Effect of 10%, 30%, and 60% body weight traction on the straight leg raise test of symptomatic patients with low back pain.J Orthop Sports PhysTher 30: 595-601.
- Wieting JM (2005) Massage, Traction, and Manipulation. Medscape.
- Werners R, Pynsent PB, Bulstrode CJ (1999) Randomised trial comparing interferential therapy with motorized lumbar traction and massage in management of low back pain in a primary care setting. Spine (Phila Pa 1976) 24: 1579-1581.
- Armstrong JR (1965) Lumbar disc lesions, (3rd edtn). Williams and Wilkins, Edinburgh, Livingstone.
- McKenzie RA (1981) The lumbar spine. Mechanical diagnosis and therapy. Spinal publications, Waikanae, NewZealand.
- Youssef J, Davidson B, Zhou BH, Lu Y, Patel V, et al. (2008) Neuromuscular neutral zones response to static lumbar flexion: Muscular stability compensator. ClinBiomech (Bristol, Avon) 23: 870-880.
- Laslett M (2009) Manual correction of an acute lumbar lateral shift: maintenance of correction and rehabilitation: a case report with video.J Man ManipTher 17: 78-85.
- McGill SM, Kippers V (1994) Transfer of loads between lumbar tissues during flexion- relaxation phenomenon. Spine (Phila Pa 1976) 19: 2190-2196.
- McKenzie RA (1972) Manual correction of sciatic scoliosis.N Z Med J 76: 194-199.
- Carroll LJ, Cassidy JD, cote P (2000) the Saskatchewan Health and Back Pain Survey: the prevalence and factors associated with depressive symptomatology in Saskatchewan adults. Can J Public Health 91: 459-464.Philadelphia Panel (2001)
- Philadelphia Panel Evidence-Based Clinical Practice Guidelines on Selected Rehabilitation Interventions for Low Back Pain. Phys Ther 81: 1641-1674.
- McKenzie RA, May S (2003) The Lumber Spine: Mechanical Diagnosis and Therapy (2nd edtn). Spinal Publications, Waikanae, New Zealand. Pellecchia GL (1994) Lumbar traction: a review of the literature.j Orthop Spotd Phys Ther 20: 262-267 Murrin KR, Rosen M (1985) Pain measurement, In: Smith G and Govindo BG (editors) Acute Pain: London: Butterworth.
- Kremer E, Atkinson JH, lgnelzi RJ (1981) measurement of Pain: Patient preference does not confound pain measurement.Pain 10:241-248.
- Revill Sl,Robinson JO, Rosen M, Hogg MI (1976) the reliability of a linear analogue for evaluating pain. Anaesthesia 31: 1191-1198.
- Vianin M (2008) Psychometric properties and clinical usefulness of the Oswestry Disability index. J Chiropr Med 7:161-163.
- Gordon SJ, Kish VL, et al. (1991) Mechanism of disc rupture. A preliminary report. Spine (Phila Pa 1976) 16: 450-456. Veres SP, Robertson PA, Broom ND (2008) ISSLS prize winner: Microstructure and mechanical disruption of the lumbar disc annulus:
- part II: how the annulus fails under hydrostatic pressure. Spine (Phila pa 1976) 33: 2711-2720.
- Donelson R, Aprill C, Medcalf R, Grant W (1997) A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine (Phila Pa 1976) 22: 1115-1122.
- Adams MA, May S, Freeman BJ, Morrison HP, Dolan P (2000) effects of backward bending on lumbar intervertebral disc. Relevance to physical therapy treatment for low back pain. Spine (phila pa 1976) 25: 431-437.
- Santolin SM (2003) McKenzie diagnosis and therapy in the evaluation and management of a lumbar disc derangement syndrome: A case study.J Chiropr Med 2: 60-65.
- Key JA, Ford LT (1948) Experimental intervertebral-disc lesions.J Bone Joint Surg Am 30A: 621-630.
- Melbye M (2010) An adherent nerve root–classification and exercise therapy in a patient diagnosed with lumbar disc prolapse.Man Ther 15: 126-129.
- Alfredson H, Pietilä T, Jonsson P, Lorentzon R (1998) Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis.Am J Sports Med 26: 360-366.
- Langberg H, Ellingsgaard H, Madsen T, Jansson J, Magnusson SP, et al. (2007) Eccentric rehabilitation exercise increases pe.
- John F.barnes,Pediatrics Myofascial release,Physical therapy forum- MRF techniques 1991
- Carol manhiann 2001.the myofascial release manual,3rd edition slack inc.
- Regi boehme,john boehme , myofascial release and its application to neuro development treatment 1991,page no.5-8,11-16,80.
- Keith Grant and Art Riggs. Modalities for massage and bodywork; Myofascial release; published by Massage Therapy Foundation 2005
- Wadell G. The back pain revolution, 2nd ed. Edinburg: Chruchill Livingstone, 2004:74
- Craig E. Morris, Low Back Syndromes,©2006,Epidemology of low back syndromes, pg 87
- Woolf A, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health
- Laura Punnett, Sc.D. et al. Estimating the global burden low back pain attributable to combined occupational exposures. American journal of industrial medicine,2005 dec;48(6):459-64
- AK Burton F;Balagué et al. European guidelines for management in low back pain; Eur Spine J. 2006 Mar;15Suppl 2:S136-68.
- Gordon Wadell. Nonorganic physical signs in low back pain;vol- 5(2),march/april 1980
- Andersson GBJ. The epidemiology of spinal disorders. The adult spine: principles and practice. 2nd ed. New York: Raven Press, 1997: 93- 141.
- Van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic non-specific low back pain: a systematic review of randomized controlled trials of the most common interventions. Spine 1997; 22:2128-2156.
- Travis Whitfill et al. Early Intervention Options for Acute Low Back Pain Patients:A Randomized Clinical Trial with One-Year Follow-Up Outcomes; J OccupRehabil (2010) 20:256–263
- Pengel LH, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: Systematic review of its prognosis. BMJ2003;327:323
- EdaGurcay et al. Acute LBP course and prognosis. Disability and Rehabilitation, 2009; 31(10): 840–845
- Christopher A Mayor; A meta analysis of massage therapy research. Psychological Bulletin Copyright 2004 by the American Psychological Association, Inc; 2004, Vol. 130, No. 1, 3–18.
- Manheim, C.J. The Myofascial Release Manual, third ed.Slack Incorporated, New Jersey, USA, 2001
- Robert Schleip. Fascial plasticity- a new neurobiological explanation: part 1; journal of bodywork and movement therapies(2003) 7(1), 11- 19.
- Paoloni J et al. Review of myofascial release as effective massage therapy technique; Athletic Therapy Today,2009,Sep;14(5):30-34
- The fascial network: an exploration of its load bearing capacity and its potential role as a pain generator, Robert Schleip, Fascia Research Project, Institute of Applied Physiology, Ulm University, Ulm, Germany
- Norkin C.C, Levangie PK, Joint structure and function, 4thed, Jaypee brothers medical publication, 2006
- I A Kapanji. The physiology of joints;2nd edition vol-3; Edinburg London &New York 1974
- John Barnes, PT. Myofascial release approach: part 1; massage magazine, dec 2006.
- Pathophysiology of pain and pain assessment. American medical association©2010
- Craig E. Morris, Low Back Syndromes, ,Myofascial release in low back syndromes,©2006 pg 243-276
- Panjabi MM 2006 A hypothesis of chronic low back pain: ligament subfailure injuries lea to muscle control dysfunction; Eur spine J 15(5): 668-76
- Schleip R, et al. 2007 Letter to the Editor concerning “A hypothesis of chronic backpain: ligament subfailure injuries lead to muscle control dysfunction” (M.Panjabi). Eur Spine J 16: 1733-35
- Paolo Tozzi.Fascial release effects on patients with non-specific cervical or lumbar pain; Journal of Bodywork & Movement Therapies (2011) 15, 405e416
- Taguchi, T., et al. The thoracolumbar fascia as a source of low back pain. In P.A. Huijing et al. (Eds.), Fascia ResearchII: Basic Science and Implications for Conventional and Complementary Health Care. Munich, Germany: Elsevier 2009
- Lieutenant Colonel Joseph R. et al. The effects of spinal flexion and extension exercises and their associated postures in patients with acute low back pain;Spine J vol20, no.21. pg 2303-2312.
- Michael Vianin DC. Psychometric properties and clinical usefulness of the Oswestry Disability Index;; Journal of Chiropractic Medicine (2008) 7, 161–163 Pedretti L W, Occupational therapy practice skills for physical dysfunction, 4thed, 1996, pg 87-88.
- Danniel&Worthighams, Techniques of manual examination, 6th edition
- Marshall P. W., Murphy BA. Evaluation and neuromuscular changes after exercises rehabilitation for low back using a swiss ball: a pilot study. Journal of Manipulative physiotherapy, 2006 sept, 29 (7) 550- 560
- D. J. L. Kuh. Height, occupation and back pain in a national prospective study; British Journal of Rheumatology 1993;32:911-916
- Michael Pfingsten. Fear avoidance behavior and anticipation of pain in patients with chronic low back pain;
- Jonathan R Field1*, Field et al. Preliminary study into the components of the fear- avoidance model of LBP: change after aninitial chiropractic visit and influence on outcome. Chiropractic & Osteopathy 2010, 18:21
- Swinkels-Meewisse IE. Fear-avoidance beliefs, disability, and participation in workers and non-workers with acute low back pain;Clin J Pain. 2006 Jan;22(1):45-54
- Hernandez-Reif M. Lower back pain is reduced and range of motion increased after massage therapy; Int J Neurosci. 2001;106(3-4):131- 45.
- Rose Adams. The Effects of Massage Therapy on Pain Management in the Acute Care Setting; Int J Ther Massage Bodywork. 2010; 3(1): 4– 11.
- Paul Dolder et al. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain;; Australian journal of physiotherapy 49: 183-188.
- www.pubmed.com
- www.google.com
LIST OF ABBREVIATION
V.A.S – VISUAL ANALOGUE SCALE
M.M.T – MANUAL MUSCLE TESTING
O.Q.D – OSWESTRY DISABILITY QUESTIONNAIRE
M.F.R – MYOFASCIAL RELEASE